Diet has hardly any effect on your cholesterol level; the drugs that can lower it often have serious or fatal side effects; and there is no evidence at all that lowering your cholesterol level will lengthen your life.
One morning in early October of 1987 the U.S. health authorities announced that 25 percent of the adult population had a dangerous condition requiring medical treatment. Since there were no symptoms, it would be necessary to screen the entire population to identify those in danger. More than half of those screened would be dispatched to their physicians for medical tests and evaluation. Then for one out of four adults treatment would begin. The first step would be a strict diet under medical supervision. If within three months the dieting had not achieved specified results that could be verified by laboratory tests, a more severe diet would be imposed. The final step for many patients would be powerful drugs to be taken for the rest of their lives…
Considering that this was expected to be one of the most important medical interventions in the nation’s history, the formal announcement was deceptively low-key. It was to be called the National Cholesterol Education Program. And while cholesterol was surely a household word, the official sponsor was less familiar: the National Heart, Lung, and Blood Institute, a major division of the federal government’s National Institutes of Health. Although the heart institute’s main job is to coordinate and finance medical research, this departure into medical intervention was not unprecedented. At first glance the program’s objective sounded positively innocuous: “To reduce the prevalence of elevated blood cholesterol in the United States and thereby contribute to reducing coronary heart disease morbidity and mortality.” But the National Cholesterol Education Program was a medical landmark in several ways. It was the culmination of an extraordinary and sustained medical-research effort targeting the nation’s biggest killer – coronary heart disease. One experiment had taken forty years and was still in progress. Another involved examining 361,622 middle-aged men. A famous experiment by two Nobel Prize winners had penetrated the innermost recesses of the human cell to identify a single gene with a dramatic effect on cholesterol levels. Researchers had studied the arteries of rabbits, given highfat diets to monkeys, and fed egg yolks to college students. It would be hard to find another medical issue that had been explored with such vigor, by so many researchers, and at such great expense. Just two important experiments took twelve years, cost more than $300 million, and consumed 60 percent of the heart institute’s clinical-research budget. There were serious risks to consider.
Not since the introduction of oral contraceptives would so many people be exposed to powerful new prescription drugs over decades. Among the most elusive hazards of any drug are damaging or even deadly side effects that are recognized only after the drug has been administered to thousands of people for years. Nor is dietary therapy quite as simple as it sounds. So complex are the interactions among food compounds, and so varied are the behavior and the chemistry of individuals, that dietary intervention has proved to be one of the most complicated of all medical treatments, subject to unexpected difficulties and disappointing results.
Finally, the National Cholesterol Education Program represented a major change in strategy in the prevention of coronary heart disease. Previous efforts, led mainly by the American Heart Association, had relied on advice and persuasion. Now the federal government was calling on the authority of physicians to prescribe a medically supervised regimen of treatment. This was not just friendly advice from the family doctor to cut down on cholesterol. It was, in the words of the treatment guidelines, a program of “behavior modification” backed by laboratory tests to ensure adherence and measure results. People still might abandon drugs that made them sick – and some cholesterol-lowering drugs were famous for doing so – or refuse to eat foods they didn’t like. But now they would be violating explicit doctor’s orders.
One would expect a government program of such importance to have survived rigorous examination and review before it moved into high gear. One would suppose that such a far-reaching intervention into the lives of millions of people had been approved by the White House and scrutinized by Congress. In fact the heart institute launched this project on its own authority, consulting panels of hand-picked specialists. One would suppose that before millions of people were put on a medically supervised diet, the diet would have been tested to demonstrate that it was safe and effective. No such tests wereconducted. One would suppose that the nation’s clinical laboratories could measure cholesterol accurately enough to identify those who needed treatment. In fact laboratory performance was so poor that millions with average or low blood-cholesterol levels would inevitably be misled into believing that their levels were dangerously high. One would suppose that before a program involving billions of dollars in doctors’ bills, laboratory tests, and medication was launched, the costs and benefits would have been carefully weighed. In fact officials refused even to guess at the total costs and had no plan to measure the benefits. And one would suppose that it had been conclusively demonstrated that lowering blood-cholesterol levels would save lives. No such evidence existed.
An Alarming Discovery
The story of cholesterol began in 1951, when the Pentagon dispatched a team of pathologists to the combat zone of the Korean War on a grisly mission to learn from the bodies of the dead. The principal assignment of the team, led by Major William E Enos and Lieutenant Colonel Robert H. Holmes, was to examine wound ballistics, and in three years the team performed autopsies on 2,000 dead soldiers. As a group, battle casualties differ greatly from the subjects a pathologist normally examines, who were mostly old and very sick when they died.
The soldiers on whom Enos and Holmes performed autopsies had been vigorous young men. So when the pathologists began to notice signs of coronary heart disease, it was surprising, because practically nobody under thirty-five dies of coronary heart disease, and these war dead were, on the average, twenty-two. So the pathologists launched a systematic study of the hearts of soldiers killed in battle. In 300 consecutive cases they dissected the single most vulnerable component of the heart – the network of tiny coronary arteries that nourish the heart muscle with blood.
These small arteries are considerably more sophisticated than hollow tubes. Their inside surface is a thin layer of very smooth, almost slick cells. The surface needs to be smooth because when the platelets and proteins in the blood encounter a break or irregularity, they lay down a deposit of fibrous material. Such a fibrous deposit on the skin is the familiar scab, and would be undesirable in an artery unless there were a leak or other damage that needed repair. The next major layer in the artery consists of smooth muscle, which can expand and contract, like other muscles in the body. One of the mechanisms by which the heart muscle can increase its blood supply is by dilating the coronary arteries, thus increasing the flow.
Enos and Holmes expected to find mostly slick interior surfaces surrounded by healthy smooth muscle. Instead they found stringy, streaky yellow deposits of fat and fiber in 35 percent of the casualties. These particular deposits had posed no immediate threat. But they meant that degeneration of the arteries was well under way more than twenty years before these men would have been likely to experience heart attacks.
In another 42 percent of the casualties the coronary arteries were in even worse shape. In this group the fatty streaks had already grown into full-fledged lesions, structures that somewhat resemble warts. Such lesions are usually capped by hard, fibrous plaque. Inside is a mass of debris that can include cholesterol compounds, dead tissue, and calcium.
Some lesions are soft, like pimples; others are rock hard. Once these lesions are established they slowly increase in size. Fortunately for human life expectancy, they can block about 75 percent of the diameter of an artery without seriously inhibiting the blood flow. Also, some areas of the heart muscle are nourished by more than one branch of the arterial network; if one artery becomes blocked, the tissue can get blood through another. One out of ten soldiers already had lesions severe enough to reduce or block entirely the flow of blood in at least one artery. Thus 77 percent of the Korean War casualties examined showed gross evidence of coronary heart disease. This was a shock to the medical community, for it meant that the process underlying coronary heart disease began much earlier than anyone had thought. Here were fully developed lesions, some entirely obstructing arteries, in twenty-two-year-olds. Furthermore, practically all the casualties showed at least some signs of coronary heart disease.
Arterial lesions would remain at the center of medical interest in coronary heart disease for decades to come. Cholesterol-lowering diets would aim to slow their growth; bypass surgery would attempt to route blood around them; in angioplasty a tiny balloon would squeeze the lesions open. In 1953, however, researchers faced a more immediate
problem. Without examining the coronary arteries directly, how were doctors going to tell who was in danger? The answer to that question was just then beginning to take shape eighteen miles west of Boston, in an industrial town called Framingham.
A Town Under Examination
if doctors could pinpoint what was different about people with coronary heart disease, maybe they could learn to save them. Tracing the development of such a universal peril would require the careful surveillance of thousands of people for years on end. One might as well examine the population of an entire town – and that is exactly the task that a team of Boston University Medical School physicians undertook, in Framingham, Massachusetts. It was among the first large-scale projects of the heart institute, which paid for and directed the study. The researchers, led by Thomas R. Dawber, hoped to recruit most of the adult residents of Framingham and study them for the rest of their lives. The project, which continues today, began in 1948.
The researchers set up shop in the mostly blue-collar community of 28,000, primarily ethnic Irish and Italians, and recruited two out of every three healthy men and women from age thirty to sixty-two. Every two years the participants would undergo physical examinations, fill out detailed questionnaires about their living habits and diet, and be tested with exercise treadmills and electrocardiographs. Probably in no other city in the United States have the population’s health, weight, and dietary, exercise, and living habits been measured so meticulously for so many years. A substantial fraction of everything that medical science knows today about the epidemiology of coronary heart disease has been learned from the residents of Framingham. But the public-health policies that have unfolded in the forty years since the study began have been heavily influenced by the strengths – and weaknesses – of the particular kind of knowledge that emerges from a study like this one.
Epidemiology is the study of the occurrence of illness. Learning who is afflicted and who is spared can help provide the tools to prevent disease, even when no cure exists and the disease process remains a mystery. Epidemiology tells nothing about whether a particular person will get a particular disease, but it may identify groups in a population which are particularly vulnerable.
However, a statistical approach can provide false clues as well as valid ones. For example, heart patients were advised to avoid coffee after researchers found a positive association between coffee and coronary heart disease. The association was misleading. The culprit proved to be cigarette smoking; smokers were simply more likely to drink coffee.
The Framingham experimenters built a detailed portrait of coronary heart disease from a sample of 5,127 adults, of whom 404 died of coronary heart disease over twenty-four years. When epidemiological studies are complete, the tidy mathematical charts and tables tend to conceal the crude and approximate character of the entire exercise. The Framingham study was no exception. Just deciding which residents had coronary heart disease involved significant amounts of medical guesswork. The typical participant failed to appear for about one out of five physical examinations. It has been hard to keep some laboratory tests uniform over so many years. While the Framingham study represents sound epidemiological research, its limitations need to be kept carefully in mind: it followed a small sample of adults selected from a single New England town nearly forty years ago. What emerged from the Framingham study was a series of risk factors for coronary heart disease which public-service advertisements, newspaper articles, books, and television talk shows have made familiar to most Americans. The two biggest risk factors could not be changed. Men were much more likely to develop heart disease than women, especially before age fifty-five. Premenopausal women were practically immune; only eleven of 1,600 such women developed coronary heart disease. Also, risk increased rapidly with age. For example, half of all deaths from coronary heart disease in the United States occur in the five percent of the population who are over seventy-four years old. But other important risk factors looked more amenable to intervention. One, high blood pressure, could be reduced directly with medication. It also appeared possible to modify smoking, obesity, and a sedentary life-style.
Among the characteristics associated with a greater likelihood of coronary heart disease, one drew special attention. People with the disease often have higher levels of an important organic chemical called cholesterol.
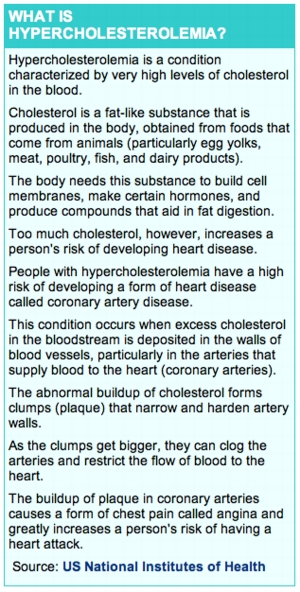
Cholesterol, as most of us know, exists in high concentrations in egg yolks, in fatty beef, pork, and poultry, and in shellfish. However, most of the cholesterol in the bloodstream is incorporated into compounds that are manufactured by the body for a wide variety of essential purposes. Cholesterol is so important that every cell in the human body can manufacture it. The membranes of cells are constructed primarily of lipids, which play a vital role in regulating what may enter and exit the cell. The body’s own chemical factory, the liver, is the largest producer and consumer of cholesterol compounds. However, the heaviest concentrations of cholesterol compounds are found in the brain. Cholesterol compounds are even essential to the manufacture of sex hormones. It is no coincidence that when all the chemicals required to form a living creature are assembled in a hen’s egg, cholesterol is a principal component.
For many years a laboratory test has been used to measure the level of cholesterol in blood serum. (Blood serum is the fluid that remains after cells and clotting agents have been removed from blood.) Since the Framingham study ranks among the most frequently cited demonstrations that high blood-cholesterol levels are linked with coronary heart disease, it is revealing to examine the evidence directly. Here is an example, calculated from the Framingham population at the twenty year point.
Average Serum Cholesterol Level Occurrence of Coronary Heart Disease
* Low (less than 200 mg/deciliter) 10%
* Average (200-239) 12%
* High (240 and above) 18%
* Average of 10 measurements over 20 years)
As blood-cholesterol levels rise, the upward trend in heart disease is unmistakable, a relationship demonstrated in other epidemiological studies. However, the same table shows extensive heart disease among those with low or average cholesterol levels. The data showed a modest relationship between cholesterol levels and heart disease. But could the researchers identify groups in the Framingham sample for whom the relationship was even stronger and more dramatic? The association was strongest, they found, in young and middle-aged men. If the analysis was limited to this group, those with high blood-cholesterol levels were three or four times more likely than those with low levels to die suddenly or have a heart attack or chest pains. Given that coronary heart disease is the nation’s single most common cause of death, this was a relationship of indisputable importance. It was to fuel scientific interest for decades to come.
 Cholesterol, however, is far from being a simple and universal explanation for what causes coronary heart disease. For example, high blood-cholesterol levels generally do not increase the risk of coronary heart disease among women. “For women there was no relationship except in the middle decade of life (ages forty to fifty ), ” Thomas Dawber, the first study director, wrote. The link between high blood-cholesterol levels and increased risk of coronary and women weakened at about age fifty and then disappeared entirely.
Cholesterol, however, is far from being a simple and universal explanation for what causes coronary heart disease. For example, high blood-cholesterol levels generally do not increase the risk of coronary heart disease among women. “For women there was no relationship except in the middle decade of life (ages forty to fifty ), ” Thomas Dawber, the first study director, wrote. The link between high blood-cholesterol levels and increased risk of coronary and women weakened at about age fifty and then disappeared entirely.
Thus, among the elderly, the group in whom most deaths from coronary heart disease occur, not appear to be a risk factor.
Another fact about cholesterol emerged from Framingham, although it was never published in deep in a typewritten report almost two feet thick, issued in 1970, is a study titled “Diet and the Regulation of Serum Cholesterol.” The Framingham researchers had for years assumed that they knew exactly why some people had higher blood-cholesterol levels than others: their diet. To measure this link they selected 912 men and women and compared the cholesterol in their diets with the cholesterol levels in their blood. To their surprise there was no relationship. Next, the researchers studied the intake of saturated fats and overall calories. None had an effect. They considered the possibility that some other factor -such as differences in physical activity – masked the effects of diet. No other factor made any difference. “There is, in short, no suggestion of any relation between diet and the subsequent development of CHD (coronary heart disease) in the study group, ” the researchers concluded in the report. It was not lost on the Framingham team that people were already being advised to diet to lower their cholesterol levels, and that more-elaborate campaigns were on the drawing board.
They concluded:
There is a considerable range of serum cholesterol levels within the Framingham Study Group. Something explains this inter-individual variation, but it is not diet (as measured here). Clearly if there is to be an attempt to manipulate serum cholesterol level in a general population it would be desirable to know what these powerful but unspecified forces are.
Among young and middle-aged men the risk of coronary heart disease did appear to rise steadily as levels of cholesterol in the blood increased. The data also showed that those with a combination of risk factors were especially prone to develop coronary heart disease, and were even more vulnerable than would be expected when the individual risk factors were added together. It was thus that the Framingham researchers and their colleagues at the heart institute emerged with mathematically elegant risk-factor equations for cholesterol, high blood pressure, and smoking.
Ways of Attack
Just as the Framingham team was refining its list of risk factors for coronary heart disease, in the late 1960s, another group of researchers was investigating ways to lower blood-cholesterol levels with diet. The troubling finding that diet and blood-cholesterol levels did not appear related was mostly ignored in the search for a specific dietary approach that might reduce the incidence of coronary heart disease.
From the previous decade’s research three competing theories emerged about how this goal might be achieved. The simplest-sounding approach was to reduce dietary cholesterol. But even crude experiments involving feeding quantities of egg yolks to volunteers demonstrated that it took huge changes in the consumption of dietary cholesterol to affect the cholesterol level in the bloodstream. The body manufactures, circulates, and uses such great quantities of cholesterol compounds that small additions or subtractions from dietary sources appeared to be insignificant. By the mid-1960s many researchers had dismissed dietary cholesterol.
Investigators also discovered that polyunsaturated fats-such as those found in corn and many other vegetable oils-reduced bloodcholesterol levels, although the mechanism by which this was achieved was not clean One approach to lowering blood-cholesterol levels through diet involved substituting polyunsaturated fats for the saturated fats found in meat and poultry. Test diets used high ratios of vegetable to animal fats. The third strategy was to reduce total calories. Not only are the overweight more vulnerable to heart attacks independent of their cholesterol levels, but the body converts any carbohydrates not immediately needed into saturated fats. This approach was based on the theory that the human body is a biochemical factory of such power and flexibility that the specific content of diet is not important within a normal range of foods.
Most of these early diet experiments shared several severe limitations. They were usually conducted in an institutionalized population for whom every aspect of diet and behavior could be completely controlled. This made experimentation easier but raised the question of whether the results would apply in the population at large. And many were limited by having a small number of participants. Diet studies quoted to this day as authoritative had as few as five subjects. If any enduring truth has emerged about human beings and diet, it is that everyone is remarkably different, and studies that don’t involve dozens if not hundreds of participants are of extremely limited value.
While these possibilities were being investigated, a peculiar thing had happened. Some health promoters – notably the American Heart Association – were already urging the public to cut down on dietary cholesterol and eat more polyunsaturated fat. Cautious voices in the medical community suggested that if it was so clear that proper diet would reduce the risk of coronary heart disease, why not prove it in an objective scientific experiment? Since the health advice they proposed to test was already being given and followed on a wide scale, this was a curious reversal of the horse and cart. It was a pattern that would occur again and again in the cholesterol saga.
Thus a team led by Ivan Frantz, of the University of Minnesota, and funded by the heart institute, began preliminary experiments for a major heart-diet trial, calling it the Heart-Diet Pilot. To make it credible and realistic, the investigators wanted to conduct it among a large group of adults living normal lives. Could they attract enough cooperative volunteers? They wanted to prove what many experts only suspected: that an acceptable and safe diet existed that would not only lower bloodcholesterol levels but also reduce the risk of heart attack. Also – and this was the hardest part – they had to learn how to monitor the food intake of thousands of adults who were conducting their lives as usual.
The team attacked each of the complicated problems . It proved possible to attract enough suitable volunteers. By creating special food warehouses where the participants could shop using specially coded cards, the experimenters were able to monitor food. Finally, they succeeded in lowering bloodcholesterol levels in a pilot test seven months long. The investigators employed all three dietary approaches, but in contrast to modern diet advice, they emphasized a diet unusually high in polyunsaturated fats. At the end of that period the blood-cholesterol levels were 10.5 percent lower than at the start. While the team had proved that blood-cholesterol levels could be lowered in a free-living population, the reductions were only about half those achieved in smaller and more limited experiments.
The Framingham study and the Heart-Diet Pilot were among the most important evidence on the table in 1971, when the heart institute convened the Task Force on Arteriosclerosis to plan some of the boldest and most expensive medical experiments ever conducted.
The Task Force set an agenda for research coronary heart disease that would guide the nation for fifteen years. Landmark policy decisions in medicine are made under ground rules and by procedures found almost nowhere else in our society; research medicine is governed by interlocking committees of elite physicians. On the first rung of the medical hierarchy are the various primary-care physicians: general practitioners, family-practice
specialists, and internists. These physicians must deal with such an enormous variety of human ailments that much of the time they can only apply hundreds upon hundreds of rules learned mostly by rote, Primary-care physicians will refer the cases that cannot be dealt with by that approach to the physicians on the next rung, the specialists. Specialists are likely to know and understand a much greater fraction of the scientific literature in their field. Their therapies may depart more frequently from what they were taught. At the top of the hierarchy are the academic faculty of medical schools and teaching hospitals. Their power reaches far beyond the fact that they train other physicians and that the most complicated cases may be referred to them. They decide when new therapies should be applied on a broad scale and when others should be abandoned. More important, this medical elite advises the Food and Drug Administration on drug safety, approves or rejects multimillion-dollar research grants, and appears on expert panels at important medical meetings. Within a specialty the club is small enough to be on a first-name basis.
Although it is a federal government agency, the heart institute interlocks tightly with this medical elite. Early in their research careers promising academic physicians often serve tours of duty as fellows at the heart institute. Later, an especially successful academic-research physician may become the director of the institute or one of its branches. Betweentimes the academic elite will sit on many official committees and co-author influential articles with institute officials. The Task Force on Arteriosclerosis that met during 1971 was an important gathering of this elite. These doctors and research scientists had not won admittance to the most exclusive club in medicine by being timid thinkers, and when they sat down to plot a scientific assault on coronary heart disease, their vision was suitably bold. In the Framingham study more than twenty years of research had gone into identifying risk factors. These results, by and large, fit in with other epidemiological evidence. Now the task force was going for the payoff: a scientific demonstration that enough was understood about the causes of coronary heart disease to prevent it. The task force remained undaunted as its various committees began the much tougher job of converting its overall mandate into detailed plans for elaborate and expensive clinical trials.
One task-force decision remains controversial to this day. Despite the elaborate Heart-Diet Pilot, the task force rejected a major trial to determine whether diet alone would reduce the risk of heart attacks, agreeing only to make diet one part of a larger trial. Task-force members concluded that the chances were too great that the trial would fail, citing two reasons. First, the cholesterol reductions expected were so small that a trial with as many as 100,000 participants, costing up to $1 billion, would be required to produce a reduction in coronary heart disease large enough to measure. Also, the task force was not convinced that dietary intake could be monitored accurately enough.
Even those who harbored concerns about the ambiguity and weakness of some of the evidence could not help being reassured by the commitment to confirming the cholesterol hypothesis through the classic scientific method. The ink was barely dry on the report of the task force before the heart institute had endorsed it and launched two of the most important medical experiments in history.
Cholesterol on Trial
The medical investigators who intended to prove that they could prevent coronaryheart disease faced a formidable task. Clinical trials are among the most elaborate, expensive, and time-consuming forms of medical research, and these experiments were going to be especially difficult. The more complicated was called the Multiple Risk Factor Intervention Trial, or MR. FIT, and itstill ranks as one of the largest and most demanding medical experiments ever performed on human beings. It took more than ten years, involved twenty-eight medical centers across the nation, employed more than 250 researchers, and cost $115 million.
Before the trial could begin, the investigators had to weigh the need for knowledge about a major threat to health against the risk that trial participants might be harmed or killed. In the most objective and convincing trials people with similar medical characteristics are randomly assigned to either a treatment group or a control group. The treatment is presumed to be beneficial, or there would be no point in the trial. But the stronger the belief that the treatment is beneficial, the more ethically troubling it becomes to deny that treatment to the control group. Would it be proper to identify thousands of men at especially high risk for coronary heart disease, assign them to a control group, and then wait to see if the predicted number died, just for purposes of accurate comparison? To resolve the problem the investigators settled on a compromise. Members of the control group would be informed that they had an above-average risk of coronary heart disease, and the results of annual physical examinations done for the sake of the experiment would be provided to their personal physicians. That solved the ethical problem, but now the experimenters worried that the untreated subjects were not a true control group, because their doctors might try to modify one or more of their risk factors. And wasn’t a routine physical examination itself a form of intervention? Nevertheless, the investigators elected to continue on the assumption that this would have little or no effect over the long run.
The average American was not the prime target of MR. FIT. Using the risk-factor equations developed from the Framingham study, the researchers were going to select for their experimental subjects those who were at highest risk from specific risk factors that they believed they understood and could control. So they excluded the elderly, who
experience the most heart attacks, and young and middle-aged women, who experience few. To get enough candidates at high risk from multiple factors required examining 361,662 men aged thirty-five to fifty-seven. The resultant group of 12,866 men was not exactly ready to run the Boston Marathon. Two thirds smoked cigarettes. Their typical diet included more than twice the recommended amount of cholesterol. Two out of three had developed high blood pressure early in life. Sixty percent were obese. Plainly, the MR. FIT trial had met an important goal: there was plenty of risk to modify. As the trial began, the men were randomly divided into two similar groups. One group was referred to the “usual care” of their physicians. The other, the “special-intervention” group, became the target of a sophisticated and sustained campaign to modify fundamental living habits.
Not only did the MR. FIT investigators have to achieve significant measurable behavior changes on a broad scale, but they had to sustain these gains over seven years. The initial strategy would be built around ten weekly group-therapy-style sessions during which the interventionists would seek to motivate their subjects to make far-reaching changes in their daily lives.
The first challenge was to lower blood-cholesterol levels through changes in diet. While the heart institute task force was unwilling to risk a pure diet trial, it did retain diet as a key component in a simultaneous assault on three risk factors. Although the relationship between diet and coronary heart disease is tenuous at best, a reasonable theory holds that dietary intervention still might work, even though the body sets a blood-cholesterol level and any cell can manufacture an additional supply. A rough analogy would be diet and obesity. It is quite possible for two people to follow exactly the same diet with one being fat and the other thin. In this instance food intake and body weight do not seem to be related. However, if both reduce their food consumption by 20 percent, both will lose weight. Such a theory might apply to diet and blood cholesterol, even though the relationship is even more indirect. The problem is that meaningful changes in diet are extremely hard to achieve and sustain. In the group sessions the participants were showered with information about specific foods, taught to shop for groceries, told how to order restaurant meals, even shown how to revise their favorite recipes. The participants were asked to record everything they ate and sign contracts pledging to abstain from various practices. In the best tradition of behavioral psychology, they were lavishly praised for each goal they attained. As measured by changes in eating habits, the behavior-modification protocol proved a huge success.
The special-intervention group cut their cholesterol intake by 42 percent, their saturated-fat consumption by 28 percent, and their total calories by 21 percent. Because nutritionists still debated which approach was the key to dietary intervention-reducing dietary cholesterol, saturated fats, or simply calories overall – the investigators touched all three bases. The interventionists had persuaded the participants to drastically alter their eating habits and sustain the alteration over years, a record that any health spa or diet clinic could envy. Sadly, the enormous life-style changes made by the participants had little effect on the level of cholesterol in their blood. The study began with the most modest of goals for blood-cholesterol levels – the 10 percent reduction achieved in the Heart-Diet Pilot. The results were a disappointment: by one measurement method blood cholesterol dropped only 5 percent, by another 6.7 percent.
Legend has it that smoking is so addictive that under early Persian tyrants even the threat of amputation of the hand did not prevent tobacco use. The interventionists’ approach was considerably more subtle but more persistent, and involved an awesome variety of techniques. Smokers received stern health lectures from physicians and heard moving personal success stories from ex-smokers. They were offered monetary rewards – the money saved by abstaining – and were taught all kinds of tricks, such as keeping cigarettes in inaccessible places, hiding ashtrays, and using relaxation techniques. At the end of four years nearly three quarters of the light smokers had quit, but only a third of those with a two-pack-a-day habit. In all, almost half the smokers quit entirely, an impressive result that substantially exceeded the study’s target. High blood pressure was the last and simplest risk factor to attack.Except in the cases of a few of the most obese men, treatment was a matter of careful periodic measurement of blood pressure and adjustment of medication as required. Eighty-seven percent of the men were treated successfully enough to push their blood pressure below the threshold that defines moderate hypertension. Two thirds reached their specific blood-pressure goal in the normal range.
The MR. FIT trial had reached an important milestone. It had demonstrated that the behavior of a large group of men without symptoms of ill health could be successfully modified, and the modifications sustained over a seven year period. The question still to be answered was how many lives had been saved. The death watch in the MR. FIT trial was as meticulously planned as the rest of the experiment.
In the special-intervention group the researchers expected to reduce the number of deaths from coronary heart disease by more than 25 percent, even after allowing for dropouts and others who wouldn’t fully adhere to the program. A panel of three cardiologists not otherwise associated with the trial evaluated each death to establish whether it was attributable to heart disease or another cause. Then, on the official record date of February 28, 1982, more than nine years after the experiment began, the investigators started to tally the results.
The trial failed completely. No significant difference in the overall number of deaths could be found between the two groups. In fact, slightly more deaths occurred among the special-intervention group. That small difference was not statistically significant – it was probably the result of chance. Considering only deaths from coronary heart disease did not change the picture. The difference between the two groups, of some 6,400 men each, was only nine deaths, also probably the result of chance.
The major surprise came in the usual-care group, the high-risk patients left to their own devices. The number of deaths from coronary heart disease was 40 percent lower than expected. Even though the usual-care group reported only minimal changes in their diet, their bloodcholesterol levels declined nearly as much as the special-intervention group’s, leaving only a two percent difference between the groups. The usual-care group did not take part in a special anti-smoking program, but 29 percent quit on their own. Although fewer of these men were treated for high blood pressure – and treatment was not pursued as aggressively as it was in the special-intervention group – the typical blood pressure in the usual care group was only four percent higher.
Among the problems the investigators faced was one that would emerge as important in other clinical trials: the results were clouded because the treatment had caused harm as well as benefit, particularly among those treated for high blood pressure in the special-intervention group. The medication not only lowered blood pressure but also raised blood cholesterol by seven percent, helping to defeat one of the other goals of the trial. The hypertension medication might also have contributed to the deaths of some of the special-intervention participants. The numbers were not large enough to be conclusive; the experimenters described the indications as “ambiguous but disquieting.”
The failure of Mr. FIT triggered a wide range of comment and criticism in the medical community, but attracted little attention in the general press. Some treatment enthusiasts tried to explain away the failure with what might be called the Physicians’ Conspiracy Alibi. Under this theory hundreds of ordinary doctors who happened to be taking care of patients in the control group secretly worked to undermine MR. FIT by providing special treatment that they did not give their other patients. Such malicious and unethical behavior by doctors scattered across the country seems very unlikely. The usual-care group proved much healthier than expected, but this was probably part of the broad decline in coronary heart disease that could be observed throughout the 1970s in all age groups across the country. A second possibility was that the Framingham study had substantially overstated the dangers of multiple risks. But one fact was clear. A ten-year, $115 million research program had demonstrated that the investigators did not know nearly as much about preventing coronary heart disease as they thought they did. The health advice given to millions of Americans over decades had been tested in a large and elaborate clinical trial, and had produced no measurable benefits.
More Attempts to Lower Cholesterol
The failure of Mr. FIT did not end the scientific drive to demonstrate that coronary heart disease could be prevented. From the start many researchers had believed that the long-sought evidence would emerge not from new behavior-modification efforts but from the classic medical intervention of drugs. However, three important requirements
had to be met. First, it had to be shown to be possible to lower blood-cholesterol levels significantly for long enough to measure the benefits, something no one had done.
Second, the cholesterol reductions, once achieved, had to be shown to reduce the incidence of coronary heart disease. The investigators were searching for a risk factor that could be modified, not just a more accurate method of identifying those most likely to die. Third, the treatment used to lower blood-cholesterol levels could not harm more people than it helped. The clearest and simplest proof of that would be showing that lowering blood-cholesterol levels prolongs life. Not only is a lower total mortality the main object but it is an important check against the possibility that intervention creates unanticipated health hazards – reducing heart attacks but causing other, unexpected problems. These were the challenges for the heart institute as its investigators drew up plans for its second large effort, known officially as the Coronary Primary Prevention Trial, or CPPT. It was launched at about the same time as MR. FIT but would take longer to complete.
One of the institute’s earlier steps in the assault on coronary heart disease had been to establish twelve special cholesterol-research laboratories, called lipid-research clinics. The importance of the subject and the prospect of a steady flow of federal grants had helped ensure that some of the clinics had been sited at universities with big names in coronary medicine, including Baylor, Stanford, Johns Hopkins, and the University of Washington in Seattle. A critical early decision was to choose a specific drug to lower blood-cholesterol levels. From among the substances available in the early 1970s the investigators selected a drug called cholestyramine, which is usually marketed under the name Questran. It reduces blood cholesterol by interfering with normal digestion. The liver manufactures a substance called bile acid, which circulates through the intestine, where it helps break down animal fats into a more usable form. When the drug is present in the intestine, it binds to the bile acid, removing it from the normal pattern of circulation. Because cholestyramine is indigestible, some of the bile acid is excreted, prompting the liver to manufacture an additional supply. Cholesterol is one of the major raw materials needed for making bile acid, and the liver obtains much of the extra cholesterol by absorbing it from the bloodstream.
The use of this particular drug gave the experiment a biochemical purity that was entirely absent from MR. FIT’s broad assault on statistical risk factors. Cholestyramine had a measurable effect on the specific cholesterol compound that was the investigators’ chief suspect. Cholesterol generally circulates in the bloodstream not in pure form but rather as an essential ingredient in a wide range of useful substances. Blood plasma is mostly water, and fats are not soluble in water. Cholesterol, with the help of proteins, combines with fats into molecules called lipoproteins. The molecules not only circulate through the bloodstream but also can pass through the delicate cell membranes, into cells throughout the body. Two of the most important cholesterol compounds manufactured by the human body are low-density lipoproteins, or LDL, and high-density lipoproteins, or HDL. These two key compounds have been popularized as “bad cholesterol” and “good cholesterol.” The exact role of HDL is not yet clear, but it appears to assist in the removal of cholesterol from cells and the blood, and is believed to be uniformly beneficial. Investigators would attack with cholestyramine what they believed to be the culprit in coronary heart disease – low-density lipoproteins. About 75 percent of all the cholesterol in the bloodstream is contained in LDL molecules. The principal effect of cholestyramine is to lower concentrations of LDL in the bloodstream. The investigators expected that the drug would reduce blood cholesterol by at least 25 percent, and LDL by even more.
Using a drug as the means of intervention also made it possible to improve the objectivity of the trial, by making it double-blind. Half the subjects would receive the real drug, and the other half an inert substance. Neither subjects nor experimenters would know who was getting the real drug and who the placebo.
The investigators intended to achieve a specific result, which they announced and published in advance. Including the modest effect of a prescribed cholesterol-lowering diet (which the investigators expected to reduce cholesterol levels by three or four percent), they expected to reduce blood-cholesterol levels in the treatment group by an average of 28 percent.
It would take at least three years before the lower cholesterol levels had any effect on coronary heart disease. After seven years coronary heart disease would have been reduced by 50 percent in the treatment group. They insisted on a rigorous statistical test to make it 99 percent certain that the results were not a statistical fluke. “Since the time, magnitude, and costs of this study make it unlikely that it could ever be repeated, it was essential to be sure that any observed benefit of total cholesterol lowering was a real one, ” the investigators explained. The process of locating 3,810 subjects for the trial took three full years and required examining 480,000 middle aged men. The researchers looked for men with extremely high levels of blood cholesterol – higher than those of 95 percent of the population. They accepted smokers in approximately their proportion in the general population, but otherwise excluded those with complicating risk factors, such as high blood pressure and diabetes. Participation was limited to men, because in this age group (thirty-five to fifty-nine) their risk of heart attack is greater. The investigators were limiting the participants to an unusual and especially vulnerable group, which greatly increased the odds of success in an expensive and demanding experiment. And yet if the experiment succeeded, questions would still remain about whether the results would have significance for the typical adult.
Even before the study began, the investigators knew they had one substantial problem, but they believed that they had dealt with it, The “harmless placebo, ” which was to be taken twice daily, consisted of eight tablespoons of a mixture of finely ground sand, sugar, and food coloring. This indigestible mixture produced moderate to severe gastrointestinal side effects in one out of four participants. And that was the placebo. The drug was worse. In the understated words of the study designers, cholestyramine is an “unpleasant drug”- so unpleasant that the design allowed for the possibility that up to 35 percent of the participants might drop out. However, the investigators vastly underestimated how difficult it would be to induce people to keep taking the drug at the prescribed dosage. It was made up of millions of tiny chemically activated resin beads in a bulk filler. In the first year of the study 68 percent of those taking it reported moderate to severe side
effects, the most common being constipation, gas, heartburn, and bloating.
The side effects might not have been so important had it not been for one unfortunate result. The investigators did not even come close to achieving the desired reduction in blood cholesterol. By the seventh year the cholesterol levels in the treatment group were only 6.7 percent lower than those in the control group. The trial’s design had called for achieving a difference more than four times as large. Two things accounted for the vast shortfall in cholesterol reduction. Although the drug appeared to absorb bile acid effectively, the liver compensated to some extent by stepping up the manufacture of cholesterol. Second, most of the participants refused to take the six packets each day that were required to achieve the full effect of the drug. So even if the hypothesis that lowering blood-cholesterol levels would prevent heart attacks was absolutely correct, the researchers had no prospect of proving it. They could not lower blood-cholesterol levels by more than a marginal amount, even under the most carefully planned clinical conditions and focusing on an ideal target population.
So the second of the important, lengthy, expensive ($142 million), and painstaking trials succumbed to the same problem as the first: there was just not enough difference between the treatment group and the control group to prove or disprove the hypothesis. Some would conclude that the experimenters were wrong about the mechanisms of coronary heart disease. Perhaps the high cholesterol levels were a condition frequently associated with the disease but not a cause. If the trials had proved anything, it was that the body has a tremendously effective mechanism for maintaining blood cholesterol levels.
It would be tempting to blame the problems of the CPPT on cholestyramine had not another trial using a different drug, suffered a similar fate. During the same period that U.S. researchers were trying to demonstrate that coronary heart disease can be prevented, an equally ambitious effort, sponsored by the World Health Organization, was under way in three European countries. The target was blood cholesterol. The drug was called Clofibrate, and the objective was to be 99 percent certain of achieving a 30 percent reduction in coronary heart disease. The prospects for bringing about this conclusive outcome dimmed quickly as it became clear that Clofibrate lowered blood-cholesterol levels by only nine percent, about half the treatment effect expected. Nevertheless, the investigators, led by the British cardiologist Michael E Oliver, achieved one promising result. While there was no difference in the number of fatal heart attacks in the group taking Clofibrate, significantly fewer nonfatal attacks occurred. But when doctors scrutinized the crucial question in all such experiments – Did the treatment group live longer? – the results were deeply disturbing.
When the trial was halted, at the end of five years, the investigators reported excess deaths in the treatment group. In the group taking Clofibrate 162 deaths had occurred, compared with 127 in a similar control group with equally high initial cholesterol levels.
The investigators spent years poring over the records trying to discover why the deaths had occurred. They documented one clear problem: “beyond a reasonable doubt” Clofibrate caused gallstones. (Three deaths had occurred during surgery to remove gallstones.) This hazardous side effect had not been reported in testing prior to the approval and marketing of the drug. Only through the careful surveillance of thousands of trial participants over two years was the side effect first documented. The remaining unexplained mortality was due to a variety of ailments, especially cancer, that affected the liver and the digestive system. In an assessment of the difficulties of preventing heart disease, the British epidemiologist Geoffrey Rose explained that “In mass prevention each individual has usually only a small expectation of benefit, and this small benefit can easily be outweighed by a small risk. This happened in the World Health Organization Clofibrate trial, where a cholesterol-lowering drug seems to have killed more than it saved, even though the fatal complication rate was only about 1 per 1000 per year.”
Among attempts to prevent coronary heart disease, Clofibrate was hardly unique in causing more harm than good. The heart institute had gained a vast amount of clinical experience from its own Coronary Drug Project, which tested four drugs on the population at highest risk for heart attacks-men who had already experienced one. One drug was estrogen, the female sex hormone, to be given to men on the theory that it might account for the dramatically lower heart-attack rates among pre-menopausal women. Barely a year into the trial the investigators stopped giving large doses of estrogen when the early results showed convincingly that this treatment caused heart attacks rather than preventing them. Three years later they discontinued giving moderate doses of estrogen after no evidence had emerged of efficacy “from the key end point of total mortality.” While estrogen apparently did not prevent further heart attacks, it frequently caused breast enlargement, atrophy of the testicles, and impotence or reduced sex drive.
The results were little more promising with the thyroid hormone Dextrothyroxine, which lowers cholesterol levels. This drug was abandoned early, when the safety monitoring committee decided that higher mortality in the treatment group was approaching the threshold of statistical significance, and that the rate of death seemed to increase steadily the longer the drug was given.
Just two drugs, Clofibrate (the heart institute conducted its own Clofibrate trial) and mega-doses of the vitamin niacin, survived the full five years of trials. Niacin looked promising in the category of nonfatal heart attacks, but it had side effects. Ninety-two percent of those taking it reported uncomfortable flushing of the skin, 49 percent itching, and 20 percent other rashes. Much smaller but statistically significant numbers reported experiencing gout, problems of the digestive system, and severe scaling and excessive darkening of the skin. At the end of the five-year trials neither Clofibrate nor niacin had affected total mortality. With the exception of estrogen, all the drugs in the trial were cholesterol-lowering agents. These were the kinds of recent results that the CPPT investigators had on hand as they began to assess the results of their own trial. This is what they found, after administering Cholestyramine daily to the treatment group for an average of 7.4 years:
A simple reading of the table suggests that the effects of treatment, if there were any, were small. The results look strongest if approached from the perspective of relative risk. While the number of deaths from all causes was about the same for the two groups, we still could say that the risk of nonfatal heart attack was reduced by 20 percent. A second and perhaps more useful approach is to look at absolute or actual risk. From this perspective we would say that more than seven years of treatment had reduced the chances of experiencing a heart attack from eight percent to seven percent.
The trial results are so meager as to raise the question of whether the cholesterol-lowering treatment had any beneficial effect. Could not these small differences be a chance result of the fact that slightly healthier patients happened to be assigned to the control group? The probability that experimental results occur entirely by chance is calculated according to a formula based on the number of participants and the size of the difference between the two groups. Two standards are widely accepted in medical research.
Under the stricter standard the effect of treatment is pronounced enough that one
can be 99 percent certain that the differences were not a result of chance – the standard proposed for CPPT. Under the less strict standard one is 95 percent certain. Ordinarily results that do not meet this 95 percent confidence test are simply discarded as “not significant.”.
Under either standard the CPPT was a failure; the small favorable trend in the treatment group was not statistically significant. If the fatal and nonfatal heart attacks were combined, the results got tantalizingly close to the more lenient 95 percent test, but still fell short. When a trial fails to meet its announced statistical standard, this is the end of the matter, and it is time to re-evaluate the theory or find another approach to treatment. However, in what was a dark hour in the heart institute’s long tradition of scientific excellence, events took a different tum. Over ten years the heart institute had spent 60 percent of its $494 million clinical-trials budget on just two efforts: MR. FIT and the CPPT. Both were bold and reasonable experiments conceived by some of the brightest minds in medical research. By the usual standards both had failed.
Instead of admitting the failure, the heart institute researchers went shopping for a statistical test that their results might pass. Deep in the fine print of statistical theory the experimenters found a more lenient standard, called a “one-tailed” test of significance, which their results would barely meet. By either a standard of common sense or the more formal rules of statistical theory, the trial results were at best marginal and at worst nonexistent. It was unlikely that even these minimal results could ever be duplicated in the real world of clinical practice. Nevertheless, the heart institute proclaimed a resounding success, perhaps borrowing the lawyers’ aphorism “When the evidence is weak, argue more loudly.”
The Journal of the American Medical Association devoted its January, 1984, issue to cholesterol, and the CPPT was featured in the two lead articles. The results, the Heart Institute authors “leave little doubt of the benefit of cholestyramine therapy.” In a conclusion that could have been an advertisement for the drug, the study report concluded, “The trial’s implications . . . could and should be extended to other age groups and women, and . . . to others with more modest elevations of cholesterol levels. The benefits that could be expected from cholestyramine treatment are considerable.” This laid the groundwork for what would become one of the largest medical interventions in the nation’s history.
The Campaign Is Launched
Like some ponderous prehistoric beast, the National Cholesterol Education Program slowly surfaced from the bureaucratic swamps of the National Heart, Lung, and Blood Institute.
The program that ultimately came into being was described in detail in 1982, in a major American Heart Association policy statement. By 1983 the heart institute was conducting detailed and expensive surveys of attitudes toward cholesterol, among physicians and members of the public, which it would use as the basis for a public-relations campaign. In late 1984 an NIH sponsored Consensus Development Conference provided the scientific mandate the heart institute had sought, and in 1985 the National Cholesterol Education Program was officially launched. In 1986 it was unveiled to the Treatment Group Placebo Group (1,906 men) (1,900 men) medical community, in 1987 to the public.
* Deaths from all causes 68 71
* Deaths from: coronary heart disease 30 38
* Nonfatal heart attacks 130 158
It is a program of vast scope and consequences. James Cleeman, the program coordinator, has said that at least a quarter of all adults would be referred to their physicians for treatment to lower their cholesterol levels. “It’s a mammoth intervention and it deserves to be a mammoth intervention.”
As heart-institute officials began to plan their anti-cholesterol campaign, it quickly became apparent that the primary obstacle was not public ignorance or apathy but the skepticism of the nation’s physicians. Owing mainly to the highly visible and unopposed news-media campaigns of the American Heart Association, the public had long ago been sensitized to the alleged hazards of dietary cholesterol. In 1983, according to a poll by the heart institute, two thirds of the public believed that a high-fat diet had “large effect” on coronary heart disease, and nearly as many believed that dietary cholesterol was an equally important hazard.
A majority of the nation’s physicians disagreed , the institute learned in a related poll. While nine out of ten thought that smoking had a large health effect, only 28 percent were equally concerned about the dangers of saturated fat, and only 39 percent about elevated blood-cholesterol levels . Therefore the nation’s doctors became the first target of the heart institute. The slogan that emerged later – “Ask your doctor about cholesterol” – would even exploit the discovery that the public had been easier to convince of the dangers of cholesterol than were the doctors who dealt with heart disease every day.
The public was largely unaware that a lively debate was being waged, mostly out of view, in the nation’s medical journals and at scientific meetings, and that expert opinion was never unanimous. In 1980, for example, Thomas N. James, then the president of the American Heart Association, had dissented on diet. “I wish to express some personal reservations about our non-exceptional advice, which is taken by the public as meaning everyone should be deeply concerned about their dietary cholesterol,” James said in a broad critique of the emphasis on diet which he delivered at the association’s annual scientific meeting. His views were reported in the American Heart Association’s medical journal, Circulation, with the disclaimer that they were not necessarily those of the association.
The heart institute’s director, Claude Lenfant, encountered stiff resistance from his advisory council, a group of influential physicians who advise on and approve research. Lenfant never asked this group to approve the National Cholesterol Education Program, because it was a “public-education program” and not medical research. But he did have to ask it to approve money for a research project to learn how most effectively to influence physicians’ views on cholesterol, especially on the diet question.
Lenfant made his request at a meeting in May of 1986. In a group generally notable for the calm of its proceedings a heated debate ensued, and in a rare rebellion the advisory council refused to endorse the director’s proposal. “Physicians just aren’t convinced (about cholesterol), ” said Eliot Corday, a prominent Los Angeles cardiologist and the council member who led the dissent. Nonetheless, the heart institute’s machinery cranked relentlessly on. Six months later the proposal was resubmitted and rejected again, after additional debate. But after another year, at a moment when the mixture of council members in attendance was slightly different, a scaled-down research program was narrowly approved. One reason for the initially low public profile of the National Cholesterol Education Program is that its primary goal was to influence the physician community.
Starting in late 1987 every practicing doctor was sent a report summarizing the institute’s “consensus” conclusions on cholesterol. A much more elaborate information kit on treatment went to 200,000 of the nation’s physicians, including cardiologists, doctors in primary care, general practitioners, internists, and family-practice physicians. The heart institute’s eager partners in promoting cholesterol consciousness are the drug companies, which are understandably excited that the government is creating their largest new market in decades. Most drugs face the inherent limitation that they soon solve the medical need that led someone to take them, and are no longer necessary. Drugs that are needed indefinitely-such as tranquilizers and medications for hypertension and angina-are the biggest money-makers. Thus the medical journals were soon packed with advertisements for cholesterol-lowering drugs, and salesmen were knocking on the doors of physicians’ offices from coast to coast. And what could be more effective in beating down physicians’ sales resistance and skepticism than the explicit endorsement of government experts?
Late last year the heart institute acquired powerful new allies. The American Medical Association, a major drug manufacturer, and two huge food companies joined forces to “declare war on cholesterol.” The public-relations and advertising campaign began to reach the public early this year and included national and local television programs,
special magazine features, cereal-box advertisements, books, videocassettes, brochures, discount coupons, and posters.
Although the effort appeared to be a public-service campaign, it was in reality a business scheme to sell products and physicians’ services. In announcing the advertising campaign to the nation’s physicians, the AMA said, “The AMAN Campaign Against Cholesterol will use national and local television to tell the public about the risks of high blood
cholesterol and the availability of cholesterol testing through your office” (emphasis added). The drug company Merck Sharp & Dohme was already aggressively marketing its new cholesterol-lowering drug, Lovastatin, under the name Mevacor. Kellogg was preparing to launch a new oat-bran cereal (Common Sense), and American Home Products to promote a cooking-oil spray (Pam) that, like almost every other vegetable oil, contains no cholesterol. The National Cholesterol Education Program guidelines suggested that treatment should not begin without a complete physical, a patient history, and a laboratory workup. This was not lost on the AMA, which noted pointedly that screening programs had found that “as many as 25% of the participants either have no personal physician, or have not seen their doctor within the past five years.” Thus a program that may have begun in sincere but misguided zeal for the public good became intertwined with greed. The world was learning how much money could be made scaring people about cholesterol. And the mainstream organizations were being joined by thousands of less responsible profiteers offering miracle treatments, wonder diets, instant cholesterol checkups, and a variety of other services and goods whose effects were nonexistent, unproved, or hazardous.
The avalanche of information reaching the public uniformly emphasized the dangers of cholesterol, but questions continued to be raised in the nation’s medical journals. From 1985, when the program was officially created, to the present, critical articles or editorials have appeared in the Annals of Internal Medicine, The Mayo Clinic Proceedings, the Journal of the American Medical Association, Medical Care, Circulation, and the Journal of the American College of Cardiology.
Although this stream of medical literature made a balanced selection of information available to the inquiring medical researcher, the opponents of the cholesterol campaign nonetheless seemed to lose ground. They conducted research or wrote an analysis, and that was the end of it. They had no money to sponsor national conferences. Their articles weren’t mailed, along with press releases, to medical writers in the popular press. Unlike the heart institute, they had no means by which to build an enormous alliance of parties with a financial or other stake in the cholesterol question. They didn’t conduct opinion polls and fund research grants to teach them how to select target audiences and influence them most effectively. Indeed, given that the heart institute is the principal source of funds for research in the field, it is a tribute to the independence of the medical community that so many physicians spoke out, and that the journals presented their views so prominently and in such detail. But the dissenters have lacked the money, skills, and perhaps even the interest to take their case to the public.
The Coalition Against Cholesterol
So far the dissenters have been overwhelmed by the extravaganza put on not just by the heart institute but by a growing coalition that resembles a medical version of the military-industrial complex. This coalition includes, first, the “authorities” – the experts in the medical schools – most of whom play leading roles in one of the twelve lipid-research laboratories established by the heart institute. Many of these researchers spent many years as principal investigators in MR. FIT and the CPPT, andtheir research establishments continue to rely heavily on heart-institute funding. Much of the rest of their funding comes from companies that manufacture cholesterol-lowering drugs.
Next is the heart institute itself. Is it possible to imagine a more effective scheme than the National Cholesterol Education Program for raising the institute’s public profile? The heart institute, in turn, is tied closely to the drug industry. Not only does it frequently test promising new drugs at no charge to the companies, but it readily endorses products it deems useful. And last comes the American Heart Association, which had long urged just such a cholesterol campaign, as part of its sometimes misdirected but long-standing efforts to modify public behavior. This coalition boasts the authority of the federal government, the money and sales forces of the drug companies , and the reach and reputation of the American Heart Association.
The entire establishment is controlled by an interlocking directorate . For example, Robert I. Levy was a lipid expert at Columbia University before helping to launch MR. FIT at the heart institute; next he directed the institute; and now he heads the research subsidiary of a drug company, Sandoz Pharmaceuticals. When the 1984 Consensus Development
Conference needed an expert to present an overview of the cholesterol problem, it invited Levy. Daniel Steinberg is a doctor and cholesterol researcher who headed the lipid-research laboratory at the University of California at San Diego. He was also a principal investigator for the CPPT, and then served on the panel that developed the details of the National Cholesterol Education Program. But his most important role was as the chairman of the Consensus Development Conference panel, which in 1984 came out strongly in favor of a national assault on cholesterol. That conference also heard from a cholesterol specialist named Antonio Gotto. Gotto was then the president of the American Heart Association, which was pushing for a campaign. He was also the head of the Baylor University lipid-research laboratory and had worked on the CPPT.
For years the American Heart Association’s leading diet expert was a Dallas cholesterol researcher named Scott M. Grundy. The consensus conference heard him as a main speaker on diet. Grundy also chaired the subcommittee that drew up the diet provisions of the National Cholesterol Education Program. His laboratory at the University, of Texas has tested cholesterol-lowering drugs.
Last November the heart institute sponsored a national conference on cholesterol, for which the chairman was John LaRosa. LaRosa heads the lipid laboratory at George Washington University. He also chairs the diet committee of the American Heart Association. He spent years as an investigator in the CPPT.
When Merck Sharp & Dohme introduced its powerful cholesterol-lowering drug lovastatin, the whole apparatus went into action. For reporters who might want a local flavor Merck helpfully provided the names and telephone numbers of nearby research physicians who would talk about the drug and identify patients, presumably for personal testimonials . It is likely that one reason these physicians consented to such an arrangement is that their laboratories were heavily involved in research funded by Merck. The Merck press release notes that in San Diego a reporter might call Daniel Steinberg; in Houston, Antonio Gotto; in Dallas, Scott M. Grundy; and in Washington, John La Rosa.
There is no reason to doubt the honesty, sincerity, and expertise of any of these men, or dozen others with multiple roles in the cholesterol establishment. The terrible danger of such a closed loop is that important and basic questions are neither asked nor answered. And that is exactly what happened when a panel of lipid researchers and heart-institute officials designed the National Cholesterol Education Program. To observe the shortcomings, consider how the program works.
What Everyone Is Told to Do
The National Cholesterol Education program divides the American public into three groups. People with serum-cholesterol levels of 240 milligrams per deciliter or more have “high blood cholesterol” and require treatment under medical supervision, by drugs or diet or both, for the rest of their lives. There is no quantum leap in risk at this level; it was arbitrarily selected to target 25 percent of the adult population. Next come those with “borderline high” cholesterol levels, defined as 200-239 mg/dl. In this group men with one additional risk factor and women with two are said to require medical treatment.
(Additional risk factors include smoking, obesity, diabetes, high blood pressure, a family history of heart disease, other vascular disease, and low levels of HDL, or high density lipoprotein.) The intent of the program’s designers to play on fear can be seen in the decision to label as “borderline-high” those levels that are actually average. Finally, those with levels below 200 mg/dl are in the “desirable” range. People in this group can be released with a lecture or a brochure about the dangers of cholesterol, and retested every five years.
Considering that treatment may prove unpleasant, inconvenient, expensive, or all three, it is obviously important to identify correctly those people likely to reap some benefit. Nevertheless, the panel that designed the National Cholesterol Education Program knew that it would result in the treatment of millions of people who had been wrongly classified.
Poor performance by clinical laboratories accounts for part of the problem. The heart institute’s lipid-research laboratories proved that serum-cholesterol levels can be measured accurately: a careful series of tests revealed an average error of one to two percent. The equipment in all twelve laboratories had been calibrated to the same reference blood sample.
This was a crucial step, because a key danger in measurement is an upward or downward bias in all results from a particular lab. The program’s laboratory standards panel set as a final target a three-percent rate of error which although it would result in some misclassification, would confine the errors to borderline cases.
Unfortunately, hardly any clinical laboratories meet this standard. The College of American Pathologists surveyed a group of laboratories and found that the error rate was, on the average, 6.2 percent. A survey last year showed that one out of five clinical laboratories had an error rate of nine percent or more. And these are the good laboratories, the 5,000 that are voluntary members of a quality-assurance program of the College of American Pathologists. Three quarters of the major clinical laboratories are not members. And the error rate in the 40,000 mom-and-pop laboratories in doctors’ offices and group practices is anyone’s wild guess.
How serious is a nine-percent average rate of error? Taking into account that some errors will be smaller and others larger than average, in most cases a person with a cholesterol level of 220 mg/dl could expect a reading anywhere from 187, deep in the “desirable” category, all the way to 267, far into the treatment group. Consider the experience of Walt Bogdanich, a Wall Street Journal reporter who sent blood samples to five different New York laboratories. He got back results that would have placed him in the high, borderline, and desirable groups. When samples from 117 Tennessee state employees were sent to a commercial laboratory, 74 percent of the employees fell into the treatment group.
Independent tests showed that only 25 percent should have been so classified. The biggest reason for the discrepancy was that the laboratory equipment accidentally inflated all the readings by approximately six percent. Such weaknesses were well known to the framers of the National Cholesterol Education Program: most of the facts presented here on error rates are taken from a report prepared for the heart institute. Basil M. Rifkind, the physician who heads the cholesterol-research branch of the heart institute, says “A lot of medicine is conducted these days in other areas where measurement is less than optimum. Holding back until you’re really satisfied would just slow things down tremendously.”.
Sloppy laboratory work is not the only problem in accurately identifying people who, according to the program, need treatment. Serum-cholesterol levels are not stable. The most detailed report on the problem comes from D. M. Hegsted, of Harvard University, who found a variation of five to nine percent in serum-cholesterol levels even among institutionalized people on a uniform diet. He estimated that taking only one measurement would result in the mis-classification of one out of three people tested. The heart-institute panel’s recommendation that at least two cholesterol measurements be taken before beginning medical treatment helps but falls far short of resolving the measurement issue.
The adult-treatment panel of the National Cholesterol Education Program inexplicably elected to create an additional and even more serious measurement problem: it based the threshold for drug therapy – the most important decision in the program – not on the simple, widely understood overall serum-cholesterol level but on the level of the LDL component. The panel decided to set the treatment-threshold level of LDL at 190 mg/dl.
The problems of measuring serum cholesterol are minor compared with those of measuring LDL. Laboratory tests for LDL are not generally available. Therefore the panel recommended that physicians deduce the level of LDL using a formula whose key component is high-density lipoprotein.
HDL can be measured, but it is present in such small quantities that the error rate is extremely high.
“Often, plasma high-density lipoprotein cholesterol measurements lack sufficient accuracy to be of practical use in an individual clinical setting,” a group of researchers from Stanford concluded in the Journal of the American Medical Association. Another survey found that in 39 percent of the labs checked the average error rate exceeded 31 percent. The fact that HDL levels vary independent of LDL adds still another source of error.
The failures of the National Cholesterol Education Program grow more severe as a patient whose cholesterol level has been classified as high proceeds with medical treatment. The initial approach calls for a cholesterol lowering diet of moderate severity, with laboratory tests at six weeks and three months to determine the results of the diet. If little change occurs, a more severe diet is imposed. The principal effect of this therapy will be to introduce 25 million adults and their families to the kind of inconvenience, frustration, and failure that medical researchers experienced in exploring the link between diet and heart disease.
Many observers in the medical community were surprised to discover that the heart institute had made diet the frontline treatment, when sixteen years earlier it had rejected a full-scale diet trial. Given the extensive scientific record on the question of diet, it is remarkable indeed to find dietary intervention once again at the center of attention. The record is replete with evidence that the link between diet and heart disease is weak, and efforts to alter cholesterol levels with diet are maddeningly complicated and fraught with peril.
The Framingham data, as noted earlier, showed no relationship between diet and serum-cholesterol levels. This means that those with high serum-cholesterol levels might well have had low-cholesterol diets, and that some of those with low serum-cholesterol levels were gorging themselves on eggs and meat. The problem was nowhere more clearly illustrated than in one of the heart institute’s own major diet studies.
The diets of 16,349 men in Framingham, Puerto Rico, and Honolulu were examined, and the subjects were followed for an average of six years. Then the diets of those who had experienced heart attacks were compared with the diets of those who had not. There was no difference between the diets in amounts of cholesterol. There was also no difference in the two groups’ consumption of saturated fats or total calories. And these similarities were found in all three geographic areas.
Only one dietary difference emerged. Alcohol consumption was 33 to 100 percent higher in those free of coronary heart disease. William P. Castelli, the current director of the Framingham study, found the likely reason for the effect of alcohol in a separate project: alcohol raises levels of HDL, or so-called good cholesterol. This discovery must have left diet researchers thoroughly frustrated. (Having spent years studying heart disease, they emerge with the advice “Have another drink.”).
“If the cross-sectional correlations among Japanese men in Honolulu and San Francisco could be translated into intervention results, ” Castelli wrote in The Lancet “a non-drinker who began drinking 5 oz. alcohol/week would accomplish as large a reduction of L.D.L. cholesterol as he could by the usually suggested lipid lowering diets.”
Castelli hastened to add that he was not serious. “This is not, and should not be taken as, a prescription for altering blood-lipids by increasing alcohol intake.
On the contrary it is a warning against too hasty modification of dietary habits on the basis of limited and poorly understood evidence.” But the diet study and the alcohol study, published in 1977 and 1981, came quite late in the game, and did little to shake a deeply held belief in the role of diet. This belief had roots in earlier research of such enormous impact that it needs to be included in any serious discussion of diet and heart disease.
The study, called “Coronary Heart Disease in Seven Countries, ” was led by one of the most energetic and prolific figures in heart research, Ancel Keys, of the University of Minnesota. He studied male Japanese farmers and Finnish factory workers, Italian peasants and U.S. railroad employees, Dutch shopkeepers, Greek island villagers, and Yugoslavian food-processing workers. When Keys put all his data together he had a striking chart in which a nation’s rate of coronary heart disease appeared to march upward in lockstep with the amount of saturated fat in that nation’s diet. In Japan, for example, both the consumption of animal fat and the incidence of coronary heart disease were a fraction of what they were in the United States.
So how are the two apparently conflicting findings on diet to be reconciled? In the Framingham study, no link can be detected between the cholesterol or saturated fat in residents’ diets and either their blood-cholesterol levels or their chances of suffering heart attack. But taken as a group, the Framingham residents consume more animal fat and also experience higher rates of heart disease than their Japanese counterparts.
An important lesson can be learned from the resolution of similar contradictions about salt and high blood pressure. The human body has a powerful mechanism to maintain a specific level of dissolved salt in the bloodstream and quickly eliminate any surplus. Therefore normal adult consumption of salt can vary over an extremely wide range without altering the internal balance. Researchers discovered that the populations of some countries, particularly certain underdeveloped nations, had diets that included much less salt than the typical American diet does. These countries also had a much lower incidence of high blood pressure. Since the American diet includes far more salt than is biologically necessary, health authorities launched a vast campaign to get the nation to cut down on salt.
Nearly two decades after limiting salt became synonymous with healthful living, the relationship was convincingly refuted. A major international research project in thirty-two nations showed that while the incidence of hypertension varied widely, salt intake had little to do with it. Only if salt was almost eliminated from the diet was there a useful effect. The life-styles and habits of millions of Americans had been changed to little or no purpose.
Where did the research go wrong? Comparisons between countries can be particularly treacherous, says William Ira Bennett, a physician and the editor of the Harvard Medical School Health Letter. “This is, at best, a tricky business, ” he says, “because you can bet that differences in salt intake are not the only differences between two such populations.” Furthermore, the researchers initially did not measure dietary salt accurately enough and did not study enough countries.
The international comparisons of cholesterol levels are probably also misleading except at the extremes. Should not comparisons of diet and cholesterol levels among thousands of similar people in one community provide more useful information than a simple comparison between two dissimilar countries? The lesson of international studies may
ultimately be that only a diet almost entirely free of animal fat and cholesterol will lower blood-cholesterol levels reliably. Partly to accommodate the American palate, more moderate cholesterol-lowering diets have been developed in an attempt to prevent heart disease. Most such diets, however, are unlikely to be effective. Only large experiments involving free-living populations give realistic estimates of the cholesterol-lowering likely to be achieved.
Here is a table of the large experiments on diet:
Cholesterol Lowering Trial Year Participants Length Effect
Heart-Diet Pilot, 1968 962 7 months 10.5%
MR. FIT, 1984 6,428 7.5 years 6.7%
Northwestern* 1986 208 6 weeks 5.2%
CPPT (diet only), 1984 3,806 7.4 years 3.5%
The Northwestern experiment also had a second phase to test the effects of oat bran. It appeared to reduce cholesterol further, but the reduction was too small to be statistically significant. Despite enormous public interest in oat bran, this seems to be the only sizable study of it amoung people on otherwise normal diets. The best result was reported in the Heart-Diet Pilot, in 1968, but this exaggerates the typical cholesterol reductions likely to be achieved today. The investigators eliminated more than a fifth of the volunteers because they were overweight, because they might have other difficulties complying with the diet, or because they might soon quit. Further, the study’s strategy, which emphasized eating large amounts of polyunsaturated fat, has since been abandoned because of concern about cancer. More realistic and typical experiences can be found in the MR. FIT and Northwestern trials, which reduced cholesterol by five to seven percent. But the investigators in these two trials had hoped to duplicate the results of the Heart-Diet Pilot, and were disappointed. The dietary results in the CPPT, in contrast, may understate the outcome of a strict diet. The diet was supplemental to the treatment under study – the drug cholestyramine – and those whose cholesterol levels responded markedly to diet were deliberately excluded.
Average cholesterol-lowering results, however, conceal the variation in the response of individuals. The HeartDiet Pilot provided the most detailed insights into individual variation. It appears that about one in seven people may prove to be diet responders, and experience blood-cholesterol reductions greater than the best average results shown in the table. Little is known about diet responders, however, including exactly how many there are and whether a strong initial diet response is temporary or can be sustained for many years. Anecdotal evidence of dramatic changes in cholesterol from diet most likely comes from diet responders, poor laboratory measurement, normal individual variation in blood-cholesterol levels, or some combination of the three. Thus those with a weak dietary response can expect cholesterol reductions of 3.8 percent or less, the lucky diet responders 10 percent or more, and the vast majority of people about five or six percent. If the evidence is absolutely clear on one question, it is that diet offers no short-term benefits; to produce a measurable effect on the slowly developing obstructions in the coronary arteries requires adherence for five to twenty years.
These facts must have been familiar to the doctors who developed the adult-treatment guidelines for the National Cholesterol Education Program. Not only are these the major studies from the scientific literature, but, again, many of the panel members were principal investigators for the two largest trials, MR. FIT and the CPPT. The guidelines repeatedly endorse diet intervention but are curiously silent about what specific results may be expected . In fact, in the only mention of an expected lowering of blood-cholesterol levels the past reductions claimed are from an unidentified metabolic ward study achieving results two to four times higher than those the heart institute actually achieved in major trials.
Equally curious was the decision to enforce diet through medical supervision. Some doctors might like the extra business, but few are trained or equipped to give the detailed dietary counseling and follow-up that are essential to achieve any results.
The final component of the program is the recommendation that millions of Americans take for the rest of their lives an expensive and unpleasant drug that the heart institute’s own elaborate tests showed had at best a marginal effect. “The drug of choice, ” according to the program’s treatment guidelines, is cholestyramine (Questran), or the chemically similar colestipol (Colestid). James I. Cleeman, the program coordinator, has estimated that one out of five people treated would ultimately be placed on drug therapy. Early reports at the American Heart Association meeting last November suggested that Cleeman’s estimate was proving accurate: in one Iowa community 19.4 percent of the people .treated were placed on drugs, in another 18.7 percent. The benefits of cholestyramine were explored in detail earlier in this article: giving the drug for 7.4 years to 1,906 men at extremely high risk of heart attack had no effect on life expectancy but did produce a favorable trend toward fewer heart attacks, though this benefit occurred on too small a scale to pass the usual statistical tests of validity. Andwhat about the costs? A total of $23 million in drugs may have prevented thirty-six heart attacks.
This works out to $647,205 per heart attack possibly forestalled. Since the heart institute now proposes to give cholestyramine to those at lower risk than the specially selected trial participants, the statistics given above exaggerate the benefits. And although different approaches to cost-benefit analysis may produce somewhat different results, the remarkable fact is that the heart institute steadfastly refused to consider the cost question in any way.
The cost issues was first raised at the consensus conference, in 1984. Robert Levy cut off a discussion about cost with this statement: “When you think about costs, think about the fact that coronary artery disease is costing sixty billion dollars. So how much is worthwhile for relieving those costs? ” Daniel Steinberg, the consensus-panel chairman, said, “I don’t think we’re trying to focus here on the costs. I think we’re here to decide what is in the best interests of the Cholesterol Lowering Trial Year Participants Length Effect
* Heart-Diet Pilot 1968 962 7 months 10.5%
* MR. FIT 1984 6,428 7.5 years 6.7%
* Northwestern* 1986 208 6 weeks 5.2%
* CPPT (diet only) 1984 3,806 7.4 years 3.5%
As to thehealth of the nation. We’ll let some other people at some other conference work that out.” But Steinberg didn’t work the problem out when he became a member of the panel that designed the treatment guidelines for the program, and in fact no one at the heart institute seems to have addressed the cost question. James Cleeman has said that not only would it be difficult to estimate the costs and benefits but it would be “inappropriate.”
What might those costs be? The most expensive component is drug therapy. Cholestyramine for five million people would cost, at current retail prices, approximately $10 billion a year. The cost of laboratory tests and physicians’ services should total $3 billion to $10 billion, and therefore the National Cholesterol Education Program should cost society $10 billion to $20 billion a year. This amount is equivalent to the total federal nutritional assistance to the poor, including food stamps. It is roughly equivalent to the cost of all federal programs to build and improve highways. It is two to three times the cost of space flight and exploration.
Some cholesterol-program officials object to comparing the indirect costs of the cholesterol program with the direct ones of federal-spending programs involving public money. The enormous costs of the program are actually more insidious. In an age of soaring deficits a $10 billion to $20 billion new federal program would face intense critical scrutiny, and severe competition from other pressing national needs. The costs of this program are better concealed but no less real. For example, at a monthly cost of $120 to $150, drug treatment may double a patient’s annual medical costs. The money for this effort will be collected primarily for the benefit of drug companies, in a scheme engineered by a small group of men and women who mistakenly believed they were doing something good.
The Dangers of Low Cholesterol
In 1974 a group of leading epidemiological researchers believed that cholesterol was going to be found guilty of another crime: an association with high rates of colon cancer. Such a trend had already been suggested by the data from entire countries – nations with diets rich in saturated fats also tended to have higher rates of colon cancer. Would people with colon cancer also have elevated blood-cholesterol levels? To find the answer, the research team assembled all the colon-cancer cases it could find among the records of men in six big epidemiological studies, including Ancel Keys’s “Seven Countries” and the men in the Framingham study.
The men with cancer did not have high cholesterol levels, as expected. They had the opposite: cholesterol levels that were lower than average for their community or country. The baffled researchers suggested that further study – among other things, a fresh look at polyunsaturated fats, or vegetable oils – was needed. They had good reason to suspect vegetable oils. A few years before, in 1971, Morton Lee Pearce and Seymour Dayton had reported in The Lancet an excess of cancer deaths in a diet trial using diets high in polyunsaturated fats. In an action that was to be repeated many times, the researchers who favored lowering cholesterol levels through diet published a rebuttal, saying that Pearce and Dayton’s results were likely a result of random chance.
However, the same relationship between low cholesterol levels and cancer was found again in 1978, in the World Health Organization’s huge trial of Clofibrate. So many cancer cases occurred in the treatment group that they outstripped any beneficial or protective effect of the cholesterol reductions. The findings raised more questions than they answered. Was it the drug or the cholesterol reductions that caused the cancer? The weight of expert opinion favored blaming the drug. Other, smaller studies linking low cholesterol levels to cancer in a variety of sites began to appear, but the authors usually dismissed what they found as “pre-clinical” indications of cancer-a matter of no great importance.
By 1980 French researchers had found the same relationship in a study of 7,603 male government employees. The incidence of cancer began to climb steadily as cholesterol levels fell below 200 mg/dl; into the range that the heart institute today calls “desirable.” The French findings did not suggest that high cholesterol levels have any protective effect against cancer. Even though the low cholesterol levels were measured and maintained for as long as seven years before the onset of cancer, the French researchers accepted the prevailing view that this was not likely to be a causal link “but in all probability reflects the advance of the clinical course of cancer.” So many investigators had found the association between low cholesterol levels and cancer that in the early 1980s epidemiological researchers began to test the customary explanation that a drop in cholesterol level was merely a by-product of cancer that could not yet be detected. In an analysis for the Journal of the National Cancer Institute, Paul D. Sorlie and Manning Feinleib went back to the Framingham data. They reported that “in some cancer cases . . . the serum-cholesterol level was lower than that expected at as much as 16-18 years before cancer diagnosis.” That made low cholesterol almost as powerful a predictor of cancer as high cholesterol was of coronary heart disease. They did not, however, regard their analysis as conclusive.
Next, in 1987 researchers at the National Cancer Institute measured the same relationship among 12,488 men and women who participated in the National Health Nutrition and Examination Survey. This was a bigger, more recent, and more representative sample of the American population than the Framingham group. The men with the lowest cholesterol levels were more than twice as likely to be diagnosed with cancer as those with the highest cholesterol levels. Further, the longer the follow-up the stronger the relationship. “It may be premature to dismiss the inverse relation between serum cholesterol and cancer simply as a pre-clinical marker of disease, ” the authors wrote in a 1987 Lancet article.
The statistical association found in so many studies neither proves nor disproves that a causal link exists between low cholesterol levels and cancer. Nonetheless, it seems plain that these findings have been unwelcome to many researchers, who have exercised an extraordinary caution that was missing from discussions of the relationship between high cholesterol levels and heart disease. It is not, however, difficult to find a theory to explain the link between low cholesterol levels and cancer. The British heart researcher Michael E Oliver asks “How much cholesterol can be depleted from cell membranes over many years without alteration of their function? ” In other words, did the membranes’ functioning become sufficiently compromised to admit carcinogens?
Cancer Is Not the Only Hazard That Has Been associated with low cholesterol. Studies from Japan raise the question of whether low cholesterol levels increase the risk of stroke. As much as American researchers have admired what seems to be the effect of theJapanese diet in keeping blood-cholesterol levels and heart-disease deaths far below those found in the United States, other effects of the Japanese diet may not be so desirable. Japan experienced far higher rates of stroke and stomach cancer than the United States did. Heart-institute researchers apparently believed that in imitating the Japanese diet they could achieve one effect without incurring the others. But some Japanese epidemiologists weren’t so sure. In the journal Preventive Medicine, Hirotsuga Ueschima and two colleagues published in 1979 a study showing that in rural communities where the average blood-cholesterol levels were below 180 mg/dl the rates of stroke were two to three times higher than those in areas with higher cholesterol levels. (The Japanese experts described the diets that produced typical serumcholesterol levels of 167 as “grossly inadequate.”) Once again heart-institute researchers greeted the unwelcome news with a torrent of objections.
In fact, the evidence is far from conclusive, in part because so little is known about the low cholesterol levels that the heart institute is aggressively pushing the American public to achieve. Despite decades of clinical trials using a multitude of strategies, the sad fact remains that none of them reduced cholesterol enough to provide an opportunity to understand either the risks or the benefits of low cholesterol levels. The trials have generally selected only subjects with extremely high cholesterol levels, and failed to alter those levels by much. The most aggressive dieting lowered cholesterol levels by only five to seven percent, drugs by only eight to ten percent.
A Powerful New Drug
The risks of low cholesterol might have remained a mostly hypothetical question had not the Food and Drug Administration in September of 1987 approved the cholesterol-lowering drug lovastatin. As one heart-institute expert put it, lovastatin looked almost too good to be true. At maximum dosage it appeared to lower cholesterol levels by nearly a third, or at least twice as much as its competitors could. Lovastatin, which is administered as small pills, presents none of the adherence problems of cholestyramine, which patients have to take every day in the form of millions of tiny indigestible plastic beads. Here at last was a drug with the potential for resolving the cholesterol controversy in a decisive manner. It was just possible that cholesterol-level changes of this magnitude might provide conclusive evidence of a capacity to save lives.
Lovastatin, or Mevacor, was approved and is now moving into widespread use without having completed any trials to measure its effect on coronary heart disease and systematically monitor potential side effects. The heart institute drew up a plan to test lovastatin among the elderly, but has so far declined to implement it. Although the heart institute is not willing to test lovastatin, it may have unwittingly become the drug’s most important promoter. The National Cholesterol Education Program does not recommend Lovastatin, because of uncertainty about its long-term safety. But it is so difficult to persuade patients to take cholestyramine that millions of people will no doubt be placed on long-term lovastatin therapy.
The experts who have evaluated lovastatin thus far have pronounced the known side effects acceptable, both in terms of the number of people affected and in severity. However, Lovastatin deserves careful scrutiny. Both the great appeal and the potential hazard of Lovastatin come from how it works. As was noted earlier, the liver is the biggest consumer and manufacturer of cholesterol compounds in the human body. Lovastatin inhibits the liver’s capacity to synthesize cholesterol. Therefore the liver must obtain the cholesterol it needs by absorbing greater quantities from the bloodstream, and blood-cholesterol levels plunge as a result.
Although Lovastatin was heralded as a revolutionary new drug when it was approved, cholesterol-synthesis inhibitors were not new, nor was earlier experience encouraging. The first such drug was called Triparanol, and it was voted by physicians the most important advance in clinical medicine in 1960. When some doctors, including Eliot Corday, the Los Angeles cardiologist, warned that it might be hazardous, they were ignored by clinicians eager for a new tool to lower cholesterol levels. Several authorities enthusiastically endorsed it. Two years later the drug was hastily withdrawn, because of severe side effects, including the rapid formation of cataracts, severe skin disorders, and heavy loss of hair. It might have become a celebrated public scandal rather than a historical footnote had not the news media’s attention been raptly focused on another drug just marketed by the same company, a drug called thalidomide.
The second inhibitor was called Compactin, and it appeared at almost the same time that Lovastatin was first being tested in lipid laboratories. The earliest journal articles on the subject often mention them together. Compactin was rapidly approved for use in Japan. Like Triparanol, it was withdrawn. The reasons for this are not known. The sole clue to compactin’s ill effects comes from Basil M. Rifkind, of the heart institute. “It was hastily withdrawn, under a veil of secrecy, ” Rifkind told the institute’s advisory council, “and no explicit statements have come out with respect to it. The problem there, however, appears to have surrounded some neoplasms (tumors) in dogs.”
One might have expected questions about the possible association between cholesterol reduction and cancer to have been raised when Lovastatin came up for approval before an FDA advisory committee. However, the most serious question raised at the committee review was whether Lovastatin might cause heart attacks rather than prevent them. That another cholesterol-lowering drug, Dextrothyroxine, caused heart attacks was not discovered until the systematic monitoring of a heart-institute clinical trial took place. Saul Genuth, one of the members of the committee that was considering Lovastatin, said in a letter to his fellow members, “The most important safety issue is that of the 12 cardiovascular deaths and 24 serious cardiovascular events recorded in approximately 1000 patients. The sponsor simply dismisses these as unrelated to drug administration.” Then, in a wry understatement, Genuth said, “If perchance, by some mechanism, the drug can itself cause myocardial infarction (heart attacks), then the benefit-to-risk ratio may be considerably lower than the sponsor projects in this application.”.
The advisory committee did not pursue the issue with Merck, perhaps because Genuth was not present at the review to press the case, and Genuth did not oppose approval of Lovastatin. The committee recommended approval of a drug intended for use over a lifetime even though the major clinical trial had lasted only twelve weeks and the long-term experience with it was limited to 200 people who had taken it for two years. Lovastatin became the most rapidly approved drug in the FDA’s history.
By mid-1988 Merck had completed a trial comparing Lovastatin with Cholestyramine and published the result in the Journal of the American Medical Association. It concluded that Lovastatin was “both more effective and better tolerated” than cholestyramine. The trial lasted only twelve weeks. In that brief time, among 176 patients taking Lovastatin, there were one fatal heart attack, two nonfatal heart attacks, and one episode of severe chest pain requiring hospitalization.
A single case of angina occurred among the patients taking Cholestyramine, The trial was too short and had too few subjects to pass normal statistical tests. But the authors of the journal article did not even comment on the suspicious number of heart attacks that had occurred.
Other fragmentary data about the adverse effects of Lovastatin continue to accumulate. The package insert warns that insomnia may be observed as an occasional side effect. In a letter to the New England Journal of Medicine one doctor noted a milder but much more frequent effect on the brain: “In our clinics we have observed no inability to sleep in patients taking Lovastatin, but 9 of 51 patients taking the drug (17.6 percent) have reported a shortening of their sleep period of from one to three hours. It is known that Lovastatin does cross the bloodbrain barrier.” If experience with animals is included, the potential long- and short-term hazards of Lovastatin include heart attacks, cancer, stroke, liver damage, cataracts, and severe muscle pain and damage.
The account presented here of the possible hazards of Lovastatin was assembled from meeting transcripts, letters, and other materials not easily available to conscientious physicians. If they wanted to learn about the risks and benefits of Lovastatin, they might have read the summary that appeared in the New England Journal of Medicine, written by Scott Grundy. In a laudatory nine-page article Grundy devotes just five paragraphs to adverse effects, concluding that drugs that work the way Lovastatin does “produce no important short-term side effects in most patients with hyper-cholesterolemia…” He warns, however, that until more is known about the drug, physicians should monitor their patients for evidence of damage to muscles and the liver.
The most important facts about Lovastatin remain unknown. There is absolutely no benefit to be gained from lowering one’s cholesterol level. No painful symptoms will disappear. No invading bacteria will be killed. Any benefits will occur over the long term and be reflected in fewer heart attacks and fewer deaths. If there are serious dangers in drastic
changes in cholesterol levels, such as heart attacks, cancer, or stroke, these too will be reflected only in the long term, and discovered only through the rigorous study of a randomized trial lasting years. The voluntary reporting of side effects to the drug manufacturer and occasional letters in the medical journals are simply not systematic or thorough enough to assess side effects. Lovastatin could be a breakthrough drugO. r, like so many previously tested cholesterol-lowering drugs, it could do more harm than good. The tragedy is that we probably won’t ever know. By late last year Merck reported that at least 350,000 people were taking Lovastatin, and it isreasonable to assume that the number climbs rapidly everyday.
The biggest long-term cost of the National Cholesterol Education Program may be the delay it entails in the search for a better understanding of heart disease. The heart institute has declared that the major cause of heart disease is elevated levels of serum cholesterol, specifically LDL.
But conflicting evidence has begun to mount. In Helsinki, Finland, a clinical trial recently succeeded in reducing fatal and nonfatal heart attacks by 34 percent and met the usual statistical tests, although, like the other trials, it had no effect on total mortality or life expectancy. The Helsinki trial is the most promising effort yet. It tested a drug called Gemfibrozil (Lopid), a chemical relative of Clofibrate, and the participants were Finnish men with severely elevated cholesterol levels. Although the Helsinki trial was a success in the battle to prevent coronary heart discase, it was also a distinct setback for the heart institute’s official view that LDL is crucial. The most powerful effect of Gemfibrozil is to raise levels of HDL, the so-called good cholesterol; it also seems to lower LDL, but its effect is not as powerful or consistent as that of Cholestyramine. (Lovastatin appears to raise HDL slightly while lowering LDL by large amounts.)
Even though Gemfibrozil was apparently twice as effective as Cholestyramine in reducing the incidence of heart attacks, the heart institute maintained its position. Rifkind, writing in the New England Journal of Medicine, was troubled by Gemfibrozil’s failure to reduce LDL. He said, “It is difficult at present to define its precise place in the treatment scheme because of its variable effects on levels of LDL cholesterol.” He urged the nation’s physicians to continue to follow the heart institute’s guidelines – or, in effect, to ignore the trial. Gemfibrozil fared little better at the FDA, where an expert committee concluded that for most patients its benefits in preventing heart disease would not outweigh its risks, which may include gall-bladder disease and cancer.
Other evidence also supports the idea that HDL is important. Framingham researchers found that HDL levels are a more accurate predictor of coronary heart disease than LDL levels. Studies of the positive effects of exercise show that the key benefit is probably the raising of HDL levels. Coronary heart disease begins to develop in young men at puberty primarily because of a sharp drop in HDL levels which does not occur in women.
HDL remains a promising frontier. But whether progress toward more effective prevention of heart disease will come through further trials of Lovastatin or through continued research into HDL, it cannot but be slowed by those who have erroneously convinced themselves that they have identified the villain.
Who Will Live Longer?
The fear of dying is what will be used to move millions of people into treatment for high cholesterol levels. The language of the cholesterol scare is simultaneously intimidating and “You are at high risk of dying of a heart attack”; “You have dangerously high cholesterol”-these are frightening words indeed. But to probe beneath such generalities is to ask a specific question: What is the actual impact on life expectancy of high or low cholesterol levels? How great a danger to life do we face? Surprising answers to these questions emerge from the same body of heart-institute research that forms the scientific basis for much of what is known about cholesterol.
The elaborate and lengthy MR. FIT trial was quickly forgotten, having failed to demonstrate that following a strict diet, quitting smoking, and lowering blood pressure prevented deaths from heart attack. However, a spin-off project was to have greater influence. A team led by Jeremiah Stamler, of Northwestern University, continued to follow the entire group of 361,662 young and middle-aged men who had originally been screened as possible participants, tallying death rates. Although the team relied on frequently unreliable death certificates and a single cholesterol measurement for each man, the sample was impressive – seventy times as large as that for the Framingham study, twenty years more recent, and consisting of residents of eighteen cities rather than a single Massachusetts town. The MR. FIT spin-off gave rise to one of the most oft-repeated slogans of the campaign for cholesterol reduction: Each one-percent reduction in cholesterol will lead to a two-percent reduction in the risk of dying of coronary heart disease.
The actual finding was the reverse: for each one-percent increase in cholesterol level, the risk of coronary heart disease increased two percent. The researchers also found no particular threshold at which the danger leaped higher-just a steady increase in the risk of dying of coronary heart disease as cholesterol levels rose. Furthermore, the 20 percent of men with the highest cholesterol levels were about three times as likely to die of heart disease as the 20 percent with the lowest cholesterol levels. The study has since become an important part of the empirical foundation for the assault on cholesterol.
The MR. FIT spin-off report, however, omitted the data needed to answer the critical question of how high or low cholesterol affects life expectancy. The answer can be deduced from a table published in a later article, about the same spin-off group, which was followed for seven years.
Serum-Cholesterol Level Dead From Living Causes Dead From Coronary From All Heart Disease
* Low (202 mg/dl or less) 97.8% 2.2% 0.5%
* Average (203-244 mg/dl) 97.3% 2.7% 0.9%
* High (245 mg/dl or more) 96.2% 3.8% 1.7%
When one looks at total mortality and not just deaths from coronary heart disease, the hazards of high cholesterol levels appear quite modest. Further, these figures apply to only a minority of those at risk: young and middle-aged men. As noted earlier, the relationship between high cholesterol levels and heart attacks is weak or nonexistent among the elderly, in whom most deaths from heart disease occur, and among pre-menopausal women, in whom the disease is rare.
An answer to the broad question of the benefits to life expectancy from lowering cholesterol levels through diet was found by a team of physicians and researchers at Harvard University. Using the risk-factor equations from the Framingham study and the diet results of the MR. FITtrial, the researchers calculated the benefits of a lifelong program of dieting. The team, led by William C. Taylor, published the results in the Annals of Internal Medicine in 1987. For persons without other risk factors, such as smoking or high blood pressure, they concluded”we calculate a gain in life expectancy of 3 days to 3 months from a lifelong program of cholesterol reduction.” Taylor and his co-authors also said that they might be overstating the benefits of cholesterol reduction, because they had assumed that no other increased risk would arise from limiting cholesterol intake and offset any reduction in the risk of heart disease.
In an accompanying editorial, Marshall Becker, of the University of Michigan, wrote, “We should make more effective and efficient use of our resources and regain public confidence by concentrating on a few areas in which deleterious effects on health are clear and profound, such as smoking prevention and cessation, alcohol and drug abuse, and gross obesity.”
The article, which was widely discussed, triggered the inevitable rebuttal from the heart institute. But Taylor’s defense was persuasive: he noted that heart-institute researchers in Framingham had just published an analysis of cholesterol and life expectancy even more pessimistic than his own. That study is equally revealing.
Four decades after the Framingham study began, the research team examined the question of total mortality and cholesterol. Again the results showed that for those with low cholesterol levels deaths from other causes mostly offset any reduced incidence of coronary heart disease. The researchers found “no increased overall mortality with either high or low serum cholesterol levels” among men after age forty-seven. There was also no relationship among women after age forty-seven, or among women younger than forty, who very rarely have coronary heart disease. Furthermore, the researchers said, people whose cholesterol levels are declining may be at special risk. “After age 50 years the
association of mortality with cholesterol values is confounded by people whose cholesterol levels are falling – perhaps due to diseases predisposing to death.” Left unanswered was how a spontaneous decline might predispose one to death while non-spontaneous response to treatment would not.
A related issue is the likely role of cholesterol in the phenomenal rise and decline in coronary heart disease. From the Second World War until 1963 the rate of mortality from coronary heart disease rose steadily and alarmingly. Then it declined steeply, throughout the 1970s and into the early 1980s. By 1986 the death rate was 42 percent lower than it had been at the 1963 peak. The cause of this enormous change has never been convincingly explained. But one factor can be ruled out: cholesterol. From 1960 to 1980 there was virtually no change in the average serum-cholesterol levels in the American population. Over twenty years cholesterol levels declined very slightly, leaving the average just three percent lower in 1980 than it had been in 1960. Even this small difference may be nothing more than a measurement error. Whatever saved so many thousands of lives – the reasons remain a mystery – it is clear that cholesterol cannot be included as an important contributor.
What the Data Really Show
The evidence on cholesterol shows: First, while the dangers of high blood-cholesterol levels have frequently been exaggerated,no evidence suggests anything desirable about levels above roughly 240 mg/dl. Among young and middle-aged men such elevated cholesterol levels have been convincingly associated with a greater riskof heart attack. But this relationship cannotbe found among the elderly, who experience a majority of the deaths from heart attack,or among women before menopause.
Because the important cholesterol compounds in the blood are synthesized inside the human body, the link between high blood-cholesterol levels and diet is tenuous and indirect. A diet rich in saturated fat, cholesterol, or calories does not necessarily lead to high blood-cholesterol levels (though it may be unhealthful for other reasons). Moderately severe dieting, even for years, does not produce a measurable reduction in the risk of dying from a heart attack, as MR. FIT, the government’s biggest trial involving diet, convincingly demonstrated. Individuals vary widely in diet response. Some can consume large amounts of cholesterol and saturated fat – or diet drastically – without producing any effect whatever on their blood-cholesterol levels. At the other extreme, about one in seven people may be highly sensitive to diet; dieting can either elevateor decrease the blood-cholesterol level of such a person by 10 percent or more.
Drugs lower blood-cholesterol levels more consistently and by larger amounts. But the drug the government now recommends – Cholestyramine – produced disappointing results when it was tested. Daily treatment of nearly 2,000 men with severely elevated cholesterol for seven and a half years may have lowered the chances of a nonfatal heart attack from eight to seven percent. And while Cholestyramine might have reduced the incidence of heart attacks, it did not improve life expectancy at all. The new drug Lovastatin achieves even larger reductions in blood cholesterol, but neither its long-term safety nor its ability to prevent heart attacks has been tested.
Laboratory reports on cholesterol are seldom dependable, because of variation within individuals and inadequate quality control in clinical laboratories. The best way to get dependable information is through repeated cholesterol measurements using a laboratory machine known to be calibrated to a standardized national sample.
For most of the people most of the time, the advice of Eliot Corday may be helpful. “Cholesterol should be checked only if there are sound clinical indications,” he wrote last February in the Journal of the American College of Cardiology. “A mixed diet low in calories and saturated fat should be recommended along with some physical exercise. . . . It is irresponsible to force the public into a costly cholesterol-reducing program without firm scientific evidence of the effectiveness of that intervention.”
The above article was drawn from Thomas J. Moore’s book, Heart Failure, published by Random House, Inc.
Source: The Atlantic, VOL:v264, ISS:n3, DATE: Sept 1989, PAGE: 37(25), ISSN: 0276-9077, ATMOA. COPYRIGHT The Atlantic Monthly Co. 1989.
The information posted above is NOT intended to replace a one-on-one relationship with a qualified health care professional and are not intended as medical advice.
Disclaimer: The entire contents of this website are based upon the opinions of each of the respective authors, who retain copyright as marked unless otherwise noted. The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Dr. Kelley and the family of researchers and writers. We, who represent Dr. Kelley and the work that he was committed to, encourage you to make your own health care decisions based upon your research and in partnership with a qualified health care professional. If you are pregnant, nursing, taking medication, or have a medical condition, consult your health care professional before using products based on this content.
If you want to use an article on your site, you have our permission to do so with proper article link and reference back to DrKelley.info. This content may be copied in full, with copyright, contact, creation and information intact, without specific permission, when used only in a not-for-profit format. If any other use is desired, permission in writing from victory@drkelley.net is required.
© Copyright 2000-2020 Kettle Moraine, Ltd. All Rights Reserved.
