New research points to bacteria in the gut linked to processed food and not eating enough fiber

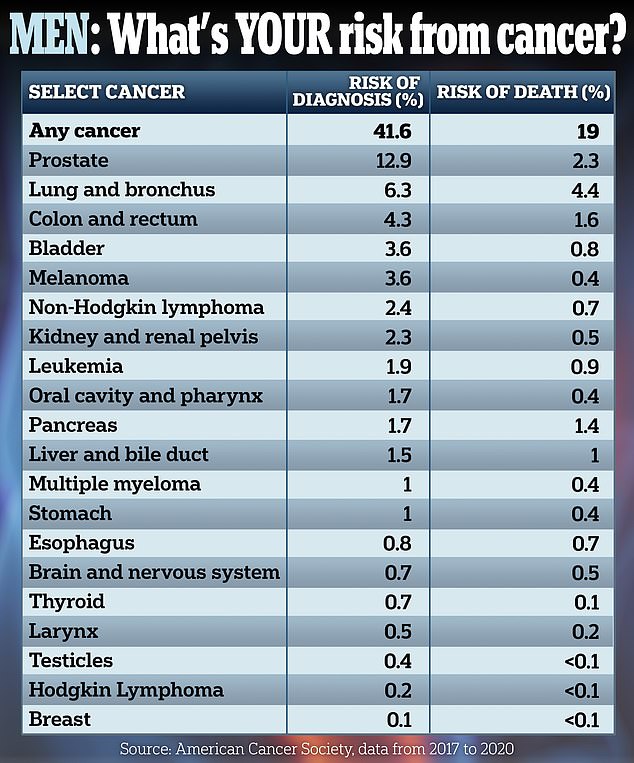
The above graphic shows the seven factors scientists say raise the risk of colon cancer in younger men
Scientists say they may be one step closer to understanding what’s driving a mystery rise in colon cancer in young people.
Researchers have discovered that patients with an aggressive form of the disease have unusually high levels of three bacteria in their guts.
Levels of fusobacterium, clostridium and shewanella have all been linked to diets high in processed foods and sugar, and low in fiber, fruit and veg.
Testing for these three bacteria could help to diagnose those most at risk, the authors wrote. It comes as colon cancer diagnoses among under-50s reach epidemic levels.
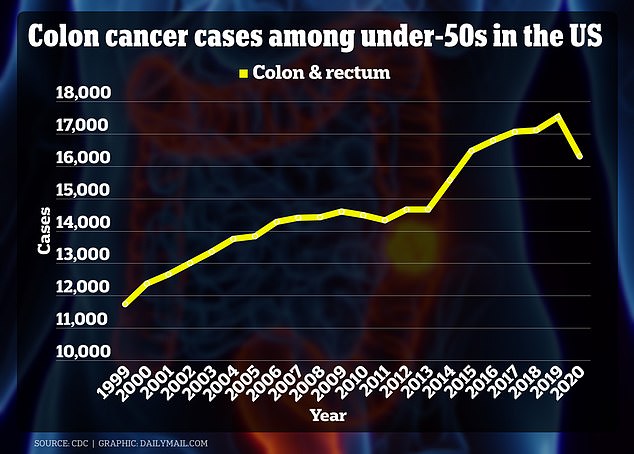
The above graph shows colon cancer cases among under 50s by year. There is a drop in 2020 because the Covid pandemic led to fewer people coming forward for screenings
Nearly 18,000 cases are diagnosed among this age group every year in the US compared to 12,000 a year pre-2000.
An even bigger rise has been seen among all cancers affecting the digestive tract, which has also been linked to poor diets.
In the study, scientists tested stool samples from 94 colon cancer patients. Twenty-four of these patients’ tumors had a KRAS mutation — which makes the cancer more aggressive.
Of the more than two dozen bacterial species they tested for, the team found three were more common among those with the more aggressive form of the disease.
Fusobacteriums can cause inflammation in the gut, the researchers warned, while Colstridium — such as C. difficile — can release toxins.
These raise the risk of damage to DNA in cells, which in turn increases the chance that they could turn cancerous.
For Shewanella, this bacteria proliferates on the surface of tumors, the team wrote — helping to support their growth.
The bacteria bifidobacterium and akkermansia were abundant in the samples from patients without a KRAS mutation.
Bifidobacterium is a probiotic that is found in yoghurt, and akkermansia has shown some probiotic activities in previous studies, including suppression of pro-inflammatory factors in the colon.
Based on this finding, the researchers speculate that the presence of these bacteria may reduce a person’s chance of developing a KRAS mutation.
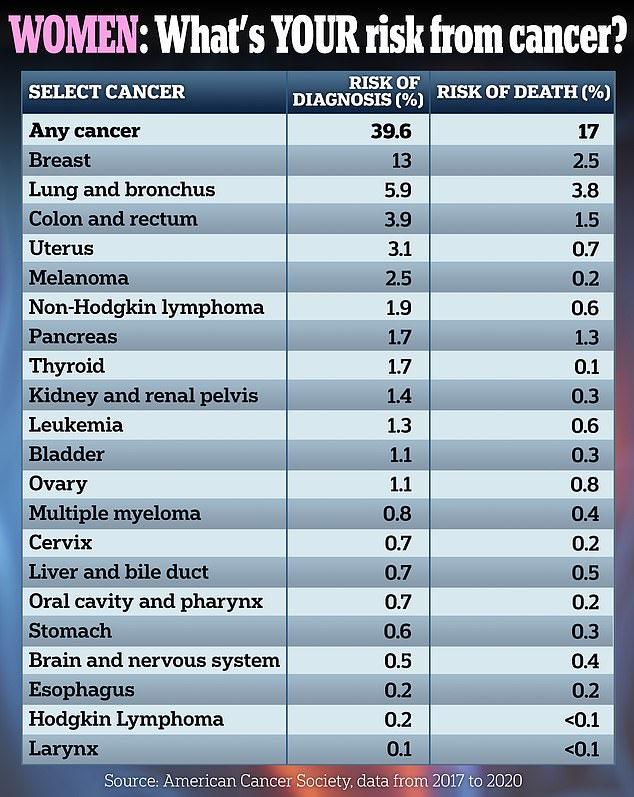
The added that it may also slow the progression of all colon cancers, which are now the number one cause of cancer deaths among men under 50 and the number two cause among women in the US.
Early-onset cancers of all forms are also on the rise, increasing by 79 percent from 1990 to 2019 globally, according to an analysis published in BMJ Oncology last year.
Scientists are stumped as to the cause of the uptick, blaming everything from antibiotics to obesity and even a type of fungus.
A $25million global probe has also been launched to attempt to track down the causes.
Young patients diagnosed with colon cancer include Evan White, 24, from Dallas whose tumor was not detected until it had progressed to stage three — when the cancer is harder to treat.
He had been on track to marry his girlfriend and move to California, but he died after a four-year battle with the disease.
Others include Marisa Maddoz, a paralegal from Delaware, who was diagnosed with the disease at the age of 29 years.
She told DailyMail.com that treatment for the cancer has left her unable to have another child.
Kate Middleton, 42, bravely revealed last month that she had also been diagnosed with cancer following abdominal surgery.
She has not revealed the type of cancer that doctors detected, but her comments prompted an outpouring of support — and inspired some cancer survivors to share their stories.
Evan White, from Dallas, was diagnosed with stage three colon cancer at the age of 24 after going into hospital to get an abscess removed from his tonsils. On the right is Marisa Maddox who was diagnosed with the cancer at the age of 29 years, She now can’t have anymore children
Previous studies have suggested patients with more Fusobacteriums in their guts consume more processed meats — sausages, bacon and jerky — refined grains — such as white rice, couscous and cornflakes — and carbonated beverages.
They also consume more red meat, such as steaks, pork chops and beef mince.
And eat less white meat, such as chicken, and fewer fruits, nuts, vegetables and beans.
For Clostridium, studies suggest people who consume high-fat diets — such as a lot of fast food — are more likely to have outbreaks of this bacteria in their gut.
This group includes the bacteria C. difficile, which causes painful blooms in nearly 500,000 Americans every year — triggering symptoms including diarrhea.
Scientists say consuming a diet low in fiber, such as lacking in grains, fruits and vegetables, raises the risk of this bacteria’s population surging in the gut.
Taking antibiotics can also cause this bacteria to proliferate, they said, because the drugs also kill off healthy bacteria in the colon.
 Revealing the study, Dr Weizhong Tang said: ‘Our new work contributes to the growing body of evidence highlighting the significance of microbiota-driven mechanisms in cancer pathogenesis.
Revealing the study, Dr Weizhong Tang said: ‘Our new work contributes to the growing body of evidence highlighting the significance of microbiota-driven mechanisms in cancer pathogenesis.
‘Understanding the specific associations between different types of KRAS mutations and colon cancer is vital.’
In the paper, published in Microbiology Spectrum, the scientists also found that Bifidobacteriums could help to prevent the progression of colon cancer.
The bacteria break down dietary fibers to produce butyrate, which has been shown to have anti-inflammatory and anti-cancer effects.
And a high population of these bacteria is linked to consuming more garlic, leeks and onions — among other vegetables.
In the paper, the researchers also revealed they had tried to make a machine learning model that could use the study results to give personalized treatment recommendations — but they said more work was needed.
Several studies have also previously suggested that imbalances in the gut microbiome could be behind colon cancer.
In one of the most compelling studies, researchers at the University of Edinburgh in the UK looked at the rates of 29 early-onset cancers — including colon cancer — across 204 regions.
In their analysis, they concluded that diets high in red meat and sodium (i.e. salt) and low in fruit and fiber were the main risks.
They also identified chronic obesity as a major factor, pointing out that it’s associated with chronic inflammation and stress to cells which can damage DNA.
Another study from January this year published in the British Journal of Cancer and based on swabs from the tumors of 1,687 people found that early-onset tumors (from patients under 45) had a different microbial profile to later-onset types.
‘A potential cause of this increasing incidence is related to changes in our gut microbiome,’ explained the lead researcher, Daniel Buchanan, an associate professor who heads the Colorectal Oncogenomics lab at the University of Melbourne.
‘Over the past few decades our diet, lifestyle and environmental factors have changed, which can alter the type of bacteria — as well as the balance between good and bad bacteria that live in our gut.’
Written by Luke Andrews for the Daily Mail ~ April 4, 2024
