Here’s Why You Should Probably Never Get One
 In 2013, the Swiss Medical Board, an independent health technology assessment initiative, was requested to prepare a review of mammography screening. The team of medical professionals included a medical ethicist, a clinical epidemiologist, a pharmacologist, an oncologic surgeon, a nurse scientist, a lawyer, and a health economist. Two of those members, Nikola Biller-Andorno, M.D. Ph. D. and Peter Juni, M.D, opened up about the project in the New England Journal of Medicine.
In 2013, the Swiss Medical Board, an independent health technology assessment initiative, was requested to prepare a review of mammography screening. The team of medical professionals included a medical ethicist, a clinical epidemiologist, a pharmacologist, an oncologic surgeon, a nurse scientist, a lawyer, and a health economist. Two of those members, Nikola Biller-Andorno, M.D. Ph. D. and Peter Juni, M.D, opened up about the project in the New England Journal of Medicine.
They said: “As we embarked on the project, we were aware of the controversies that have surrounded mammography screening for the past 10-15 years. When we received the available evidence and contemplated its implications in detail, however, we became increasingly concerned.”
In 2016, it is estimated that approximately 246,660 new cases of invasive breast cancer will be diagnosed in women in the United States as well as 61,000 new cases of non-invasive breast cancer. Mammograms continue to be touted as the most effective screening tool we have today to find breast cancer.
However, these two doctors were shocked to discover that there is minimal evidence that actually indicates that the benefits of mammography screening outweigh the harms.
“The relative risk reduction of approximately 20 percent in breast-cancer mortality associated with mammography that is currently described by most expert panels came at the price of a considerable diagnostic cascade, with repeat mammography, subsequent biopsies, and over-diagnosis of breast cancers — cancers that would never have become clinically apparent.”
The Canadian National Breast Screening Study, which was conducted over the course of 25 years, concluded that 106 of 484 screen-detected cancers were over-diagnosed.
The doctors explained: “This means that 106 of the 44,925 healthy women in the screening group were diagnosed with and treated for breast cancer unnecessarily, which resulted in needless surgical interventions, radiotherapy, chemotherapy, or some combination of these therapies.”
The fact that the benefits of this form of cancer screening are so overestimated seems worrisome for the medical community and patients at large. How, in this day and age, do we not have more awareness, more answers, and better technology?
Another review of 10 trials involving more than 600,000 women discovered no evidence that mammography screening was effective on overall mortality. This caused concern over the benefits of the medical practice. A survey of U.S. women’s views on the mammography screenings discovered that 71.5 percent of women think that it lessened risk of death from breast cancer by half, while 72.1 percent believed that 80 deaths could be avoided per each 1,000 women screened. Their perceptions were gravely over-calculated. In fact, when looking at the real numbers, mammography results in a risk reduction of 20 percent and only 1 death can be prevented per 1,000 women screened.
The Swiss Medical Board report became public in February 2014, provoking the board to advise that the quality of mammography screening ought to be evaluated and that women should be educated about both the benefits and the harms of the medical practice.
The report created controversy within the Swiss medical community, even though it supports a growing perspective around the world that mammography for breast cancer screening in asymptomatic populations is outdated and harmful at best.
When reviewing the data in regards to every breast cancer death prevented in U.S. women over a 10-year period of yearly screening starting at the age of 50, you will find that:
- 490-670 women usually have a false positive mammogram with repeat examination
- 70-100 women usually have an unnecessary biopsy
- 3-14 women were the victim of over-diagnosed breast cancer that would never reach clinical relevance
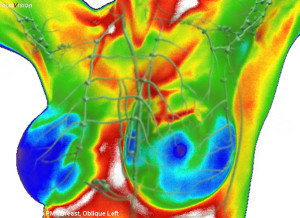
Furthermore, up to 50 percent of women have breast tissue that is dense. This makes it very hard to read mammograms correctly, as dense breast tissue and cancer both show up white on an X-ray.
Due to the lack of evidence in support of mammography and the clear potential risks involved with them, the board chose to recommend cancelling mammography-screening programs altogether. Although their recommendations are not legally binding, the report caused an uproar amongst Swiss cancer experts and organizations. The doctors on board reported:
“One of the main arguments used against it was that it contradicted the global consensus of leading experts in the field… Another argument was that the report unsettled women, but we wonder how to avoid unsettling women, given the available evidence.”
It’s clearly no mystery why the board become increasingly concerned about their researcher. The “evidence” simply does not back up the global consensus of other experiences in the field suggesting that mammograms were safe and capable of saving lives.
When it comes down to it, we are dealing with outdated clinical trials, the benefits do not clearly outweigh the harms, and women’s perceptions of mammography benefits do not match reality,
More Information On Breast Screenings
I believe that if you did have a tumor, the last thing you would want to do is crush that tumor between two plates, because that would spread it. – Dr. Sarah Mybill, General Practitioner (taken from the documentary trailer below)
I think if a woman from the age of 50 has a mammogram every year, or every two years, she’s going to get breast cancer as a direct result from that. – Dr. Patrick Kingsley, Clinical Ecologist (take from the documentary trailer below)
In 2011, 220,097 women and 2,078 men in the United States were diagnosed with breast cancer, and 40,931 women and 443 men in the United States died from breast cancer. It has become the most common type of cancer among women.
Below is a trailer to a documentary entitled, “The Promise.” The film interviews various researchers, scientists, doctors (and more), all of whom are hoping to shed light on a practice which is turning out to be not only useless, but harmful to those taking part. There is more information below the video, but I highly recommend you watch the documentary.
There is a wealth of scientific data concluding that mammograms are not, as the CDC claims, the most effective way to detect breast cancer. In fact, having a mammogram is likely the last thing you want to do if you have breast cancer.
A study published in The European Journal of Public Health titled “Trends in breast cancer stage distribution before, during and after introduction of a screening programme in Norway” found that breast screenings actually increase the incidence of localized stage cancers without reducing the incidence of advanced cancers.
The study, which used a huge population sample of 1.8 million Norwegian women diagnosed with breast cancer from 1987 – 2010, found that:
“The annual incidence of localized breast cancer among women aged 50–69 years rose from 63.9 per 100 000 before the introduction of screening to 141.2 afterwards, corresponding to a ratio of 2.21 (95% confidence interval: 2.10; 2.32). The incidence of more advanced cancers increased from 86.9 to 117.3 per 100 000 afterwards, corresponding to a 1.35 (1.29; 1.42)-fold increase. Advanced cancers also increased among younger women not eligible for screening, whereas their incidence of localized cancers remained nearly constant.”
 This study outlines how Norway’s breast screening program has actually increased the chance of being diagnosed with early stage breast cancer by more than 200%, as well contributing to an increased chance of receiving advanced stage breast cancer diagnosis by 35%. This is the opposite of what mammograms are supposed to do; if they were useful then the incidence of cancers would be lower and not higher.
This study outlines how Norway’s breast screening program has actually increased the chance of being diagnosed with early stage breast cancer by more than 200%, as well contributing to an increased chance of receiving advanced stage breast cancer diagnosis by 35%. This is the opposite of what mammograms are supposed to do; if they were useful then the incidence of cancers would be lower and not higher.
The study concluded that:
Incidence of localized breast cancer increased significantly among women aged 50–69 years old after introduction of screening, while the incidence of more advanced cancers was not reduced in the same period when compared to the younger unscreened age group.
It’s important to note that, “although the study did measure the impact of Norway’s breast screening programme, a comparison of trends between participants and non-participants in the age group eligible for screening warrants further investigation. Also the causal link between stage distribution and mortality needs to be investigated in the context of screening.”
A paper published in 2011 in the British Medical Journal set out to prove that breast screening by mammography is associated with a steeper fall in mortality cancer compared to other countries who were not offering this service. They did not expect to find the complete opposite; they found a drop in breast cancer mortality among women who were not screened. They concluded that the recent downward trend in breast cancer mortality had nothing to do with screening and everything to do with improvements in treatment and service provision.
“The new data published in the BMJ now suggests that none of the gratifying falls in breast cancer can be attributed to screening and that the very existence of a NHSBSP (national breast screening programme) should be questioned. Unless there is public pressure for an independent inquiry to challenge the status quo, it will be business as usual for the screening programme. Furthermore, the Department of Health has painted itself into a corner and it is no longer a question of scientific debate – the subject has become too politicized by those who like to avoid U-turns at all costs.” – Michael Baum, Professor Emeritus of Surgery and visiting Professor of Medical Humanities at University College London, is a leading British surgical oncologist who specializes in breast cancer treatment.
This would be an asymptomatic woman walking along the high street, having a mammogram, and then two weeks later she’s told she has to have a mastectomy. This is so cruel that it should make you weep. (quote taken from the documentary trailer above)
As Sayer Ji, founder of Greenmedinfo.com points out, a National Cancer Institute commissioned expert panel concluded that “early stage cancers” are not cancer, they are benign or indolent growths. This means that millions of women were wrongly diagnosed with breast cancer over the past few decades and have been subjected to harmful treatment, when they would have been better off leaving it untreated or diagnosed; frighteningly, it is not uncommon for a breast cancer misdiagnosis to occur.
Another study that was recently published in the British Medical Journal concluded that regular mammogram screenings do not reduce breast cancer death rates. And they found no evidence to suggest that mammograms are more effective than personal breast exams at detecting cancer in the designated age group. The study involved 90, 000 Canadian women and compared breast cancer incidence and mortality up to 25 years in women aged 40-59.
The study was conducted over a period of 25 years.
Many Studies Showing The Same Thing
The sheer number of studies that have been published on breast mammography examinations and their failure to produce a benefit in screened populations is overwhelming. What’s even more disturbing is the fact that these types of examinations have also been shown to increase the risk of breast cancer, and to have negative implications for both physical and mental health.
“U-turns do not embarrass clinical scientists, unlike politicians: if the evidence changes then our mi”nds must change. As the national programme began to run its course, two disturbing observations made me begin to question my original support. First, about 10 years after the initiation of the service, updated analyses of the original data set by independent groups in Europe and the US found that the initial estimate of benefit in the reduction of breast cancer mortality was grossly exaggerated.” – Michael Baum, Professor Emeritus of Surgery and visiting Professor of Medical Humanities at University College London, is a leading British surgical oncologist who specializes in breast cancer treatment
Researched by and published on Get Cancer Cure ~ October 8, 2016.
 FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of environmental, political, human rights, economic, democracy, scientific, and social justice issues, etc. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U. S. C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. For more information go to: http://www.law.cornell.edu/uscode/17/107.shtml“
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of environmental, political, human rights, economic, democracy, scientific, and social justice issues, etc. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U. S. C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. For more information go to: http://www.law.cornell.edu/uscode/17/107.shtml“
