Despite its reputation as an illness of the past, the deadly disease is as much of a threat to people in America as Ebola and Zika.
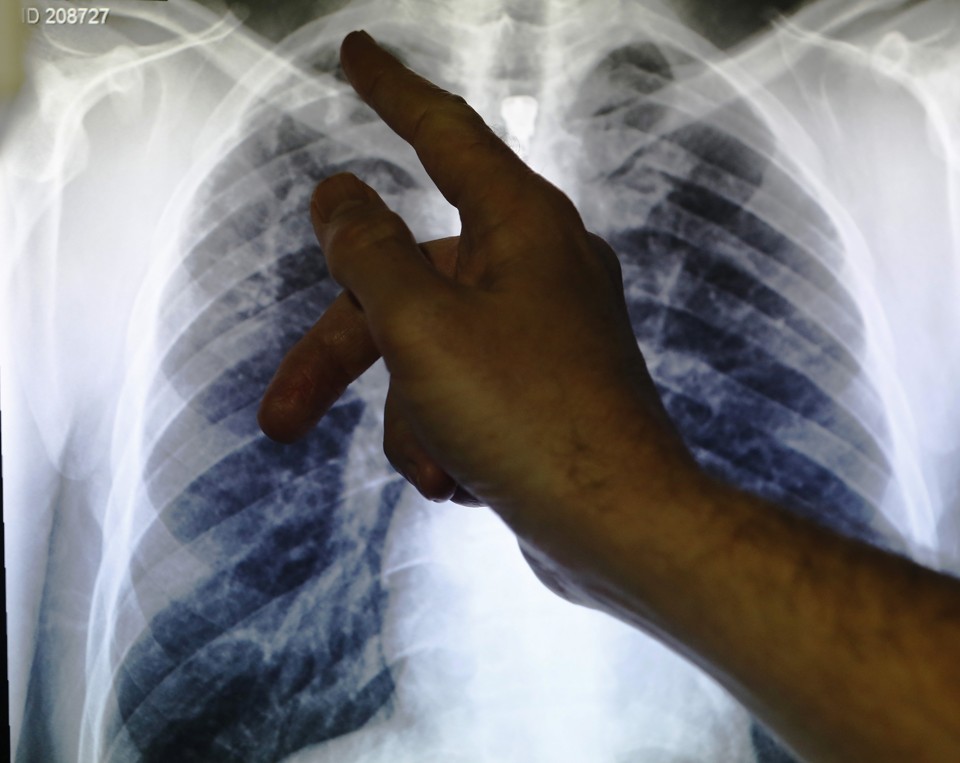
An X-ray showing a pair of lungs infected with tuberculosis. Luke MacGregor / Reuters
A century or so ago, tuberculosis was everywhere. It killed babies and brides, firemen and heads of state. The colloquial term of the era, “consumption,” littered the obituary pages and underscored how ubiquitous the disease was. Tuberculosis was so pervasive it eventually consumed you.
Actually, “consumption” got its name from the severe weight loss that so many of the afflicted suffered. The other 19th-century nickname for tuberculosis was even more evocative: “the white plague,” on account of the ashen complexion of its victims.
The novelist Charles Dickens wrote of tuberculosis in 1838 as “a dread disease” which “medicine never cured,” and which “wealth never warded off.” An illness “in which death and life are so strangely blended, that death takes the glow and hue of life, and life the gaunt and grisly form of death.” Health officials once predicted tuberculosis would be eradicated by 1915. They were wrong. Yet in the United States, where tuberculosis has been on the decline since 1992, there’s a vague perception that it is a historic disease—long since cured and largely forgotten.
That is not the case.
Tuberculosis remains a major killer. As antibiotic-resistant strains of the disease spread across the globe, it’s getting harder to wipe out. In the next three decades, drug-resistant strains of the bacteria could drive up tuberculosis deaths by 2.4 million per year—to some 4 million fatalities annually—according to a report published last year by the Review on Antimicrobial Resistance.
“In fact, tuberculosis is now the leading cause of death from infectious disease worldwide,” Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases, told me. “It is understandable—though not excusable—that people in the United States think this is not really a problem. Most of the time people don’t think beyond our borders.”
* * *
Of the nearly 10 million people who get tuberculosis every year, some 1.5 million people die. And although the death rate among tuberculosis patients has plummeted since the 1990s, the rate of the decline is slowing as drug-resistant forms of the illness create new challenges for treatment. These days, half-a-million people are sickened with antibiotic-resistant tuberculosis each year, a statistic that David Perlin, the executive director of the Public Health Research Institute at Rutgers University, calls the “most troubling” aspect of an already deadly disease. “We cannot delude ourselves into believing that TB has gone away in the USA…” he told me in an email. “It always looms large.”
Now, scientists and doctors are scrambling—with relatively little public research funding to support them—to prevent a catastrophic scenario in which antibiotics stop working on tuberculosis altogether. “Decades ago, before there was a a lot of multiple- and extensive-drug-resistant tuberculosis, we would be able to treat it no problem,” Fauci told me. “But what we have now is the danger that if one does get infected it is a very, very difficult disease to treat.”
“Sooner or later, when you do that, it comes back to bite you.”
To understand the emergence of drug-resistant tuberculosis, it helps to begin with the global distribution of the disease in 2016. About 2 billion people worldwide are already infected with tuberculosis, including 13 million people in the United States. The “overwhelming majority” of them have what’s called latent tuberculosis: meaning, they’re carriers of the M. tuberculosis bacteria, but they aren’t infected with—nor can they spread—the disease.
Still, people with latent TB are at a higher risk of acquiring active tuberculosis at some point in their lifetimes; about a one-in-10 chance overall, Fauci says. Other groups, like people with HIV and other immunosuppressed patients, are also at a higher risk of infection.
In general, tuberculosis is spread through human-to-human contact and through the air, when someone who’s infected coughs or sneezes. But there are two main ways that people get sick with drug-resistant TB. The first way is that people who are sick with tuberculosis fail to take a full course of antibiotics, and the bacteria develops a resistance to drugs that would otherwise knock it out. The second way is that a person is infected with a strain of the bacteria that’s resistant to antibiotics to begin with. (Extensively drug resistant TB, sometimes called “total drug-resistant TB,” is an even more severe category of multi-drug resistant TB.)
Drug-resistant tuberculosis in the United States is still quite rare. There were 91 such cases in the U.S. in 2014, according to the Centers for Disease Control and Prevention. But foreign-born people in the United States are much more likely to have drug-resistant tuberculosis than those born in the United States; 88 percent of the U.S. cases of antibiotic-resistant tuberculosis in 2014 were among foreign-born patients. These figures are meaningful especially in a country where immigrants face deep discrimination from wide swaths of the population.
“For the United States, the challenge is probably people coming in from immigrant populations who are already stigmatized,” said Glenda Gray, the president of the South African Medical Research Council and an expert on tuberculosis and HIV. “You need an environment that’s not going to be punitive [to care for] the people that are the refugees, the people that are on the fringes of society, and the people who are less educated.”
Drug-resistant tuberculosis is a huge problem in South Africa. Although the precise number of cases is unknown, public health officials estimate that, of the hundreds of thousands of people who develop tuberculosis in the country each year, tens of thousands of them have drug-resistant strains. (Like South Africa, India, China, and several countries in eastern Europe are considered “high burden” areas for their outsized populations of patients with antibiotic-resistant TB, according to the World Health Organization.) The true number of those who have the disease may be much larger.
In South Africa, for instance, mineworkers are at an exceptionally high risk of catching and spreading tuberculosis due to overcrowded working and living conditions and prolonged exposure to poorly ventilated workspaces. But mine workers are also less likely to have or seek access to effective treatment for the disease. Some of them may be unaware that they have the disease, or they may resist being tested for fear of losing their jobs.
“We don’t have enough drugs to help us. For TB, we’re running out of options.”
“You’re not going to have people jumping up and down saying, ‘Test me! Test me!’” Gray said. “It’s a very complex social issue that you have to address. Particularly in America, you’re going to stigmatize an already-stigmatized community, so how do you raise awareness without stigmatizing people?”
Antibiotic resistance only complicates an already daunting public-health crisis. “We don’t have enough drugs to help us,” Gray said. “For TB, we’re running out of options.”
Medicine to treat tuberculosis has existed for decades, but it hasn’t changed much in that time. In order to be effective, a course of antibiotic treatment lasts for a full year, sometimes two, an unusually long duration that researchers in a 2007 PLoS Medicine paper described as a “fundamental problem” in tuberculosis treatment. The drugs that work are toxic to the person taking them, which makes the side effects particularly grueling.
“Oh my God, it’s terrible,” said the physician and humanitarian Paul Farmer, who has written extensively on community-based healthcare models as a way to quell the spread of drug-resistant tuberculosis and other diseases. “It’s awful. It’s been 40 years since we’ve had new drugs. It’s so sad.”
Farmer calls the lack of community-based care the “Achilles heel” of the health care system in the U.S., which incentivizes frequent and costly hospitalizations for patients with TB and other chronic diseases who have few other options for care. “They get bounced in and out of hospitals or halfway houses, where if they had a community health worker checking in on them every day, you always see decreased use of emergency rooms.”
The idea behind community-based care is to set up a system where nurses and other workers visit people who need care each day, encouraging them to take medicine, taking vital signs if necessary, and so on. Eligible patients for such visits might be people who have HIV, TB, mental illness, or diabetes, he says. For tuberculosis specifically, Farmer says, community-based care would help people stay on course with their antibiotics; a crucial component of keeping drug-resistant TB at bay. “Without community-based care, I don’t see how it can work,” he said. “There’s not a lot of evidence that anything else works. It costs a lot more to give bad care in a facility than to give good care with community health workers.”
At the same time, Farmer, Gray, Fauci, and other public health leaders emphasize the need for an infusion of research funding for development of new and better medicine to treat tuberculosis. The Bill and Melinda Gates Foundation has donated tens of millions of dollars in grant money to pursue a tuberculosis vaccine, but public funding for such research is scant. TB is now a “standout poor performer” compared with research focused on “most bacterial infections, parasitic infections, and viral infections,” Farmer told me. Meanwhile, existing drugs may become obsolete due to antibiotic resistant strains of the disease. “You’re facing the valley of death because there’s nothing on the horizon.”
Given the link between HIV and TB—a huge proportion of HIV deaths are linked to TB, as people living with HIV are up to 30 times more likely to develop active tuberculosis than people without HIV—scientists often point out how much better HIV researchers have been at securing funding for fighting that disease.
“All the things that we have with HIV are in stark contrast to what we have with TB,” Fauci told me. “With tuberculosis, we don’t have a good way to monitor the disease, we don’t have good biomarkers, we don’t have good ways to figure out the efficacy of treatment.”
In other words, there’s urgent need not just for newer drugs with less burdensome treatment regiments; but also a need for a faster way to diagnose TB, and drug-resistant TB in particular. But it may be impossible to secure financing for such efforts in a public funding environment in the United States that is, many scientists told me, grossly isolationist. (See also: The Congressional failure to fund Zika research.) The United States, as a wealthy country, has a “moral obligation” to take action, Fauci says, but investing U.S. dollars in the fight against tuberculosis is also a practical matter of protecting Americans.
“We can’t say, ‘Because this is a problem somewhere else, we can’t or shouldn’t make major investments,’” Fauci told me. “Sooner or later, when you do that, it comes back to bite you.”
Gray, the physician in South Africa, says the planet’s “only hope” of someday eradicating tuberculosis rests with the United States, an affluent nation where cases of the disease are, for now, contained among small and somewhat predictable portions of the population. But global eradication of tuberculosis is a pipe dream too far off to even consider seriously, several scientists told me. The first step is to get the disease—and drug-resistant strains of the bacteria—under control, and to do so quickly. Before things get worse.
“It’s a shame,” Farmer said, “because the history of tuberculosis control is really one of forgetting. This is a transnational disease. So is Zika. So is Ebola. Without investments in the health system, the dream of rounding those last cases up? It’s really not a good dream. It’s more like a nightmare.”
Written by Adrienne Lafrance and published by The Atlantic ~ August 3, 2016.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of environmental, political, human rights, economic, democracy, scientific, and social justice issues, etc. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U. S. C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. For more information go to: http://www.law.cornell.edu/uscode/17/107.shtml“
