
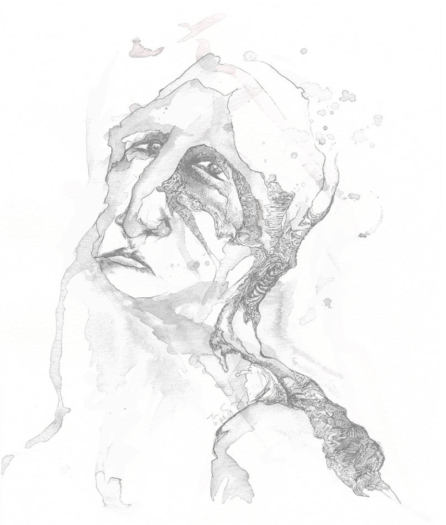
Artwork by Talia Goldenberg
After enduring years of painful headaches and injuries, Talia Goldenberg — a lively, uninhibited artist — was ready for surgery to help stabilize her flexible spine.
3:46 p.m. Feb. 10, 2014
Talia Goldenberg emerged from the fog of anesthesia. The 23-year-old wiggled her toes. She wagged her feet. Good signs for a patient coming out of spinal surgery.
The doctors at Swedish’s Cherry Hill hospital declared Talia’s surgery a success. Her surgeon noted there had been no complications and told her parents it had been “perfect.” The medical team talked about perhaps presenting the case so others could learn from the work.
It was just the news Talia and her parents had sought when they traveled from Oregon to Seattle for a promising elective surgery at the hands of one of the nation’s most prominent neurosurgeons, Dr. Johnny Delashaw. He was a star at Swedish, celebrated in ads for his workload of 350 spine procedures per year, along with many additional surgeries for aneurysms and tumors.
That volume of cases is meant to reassure prospective Swedish patients. After all, who wouldn’t want a surgeon who has seen everything?
But as the anesthesia faded in Talia’s system, she realized that not everything was perfect, despite the confident assurances of her surgical team.
Her lower jaw was ajar, jutting forward like a bulldog’s. Her face was swollen. Her delicate, singsong voice came out in a harsh rasp. She couldn’t open her mouth enough to squeeze in a finger. On her hospital bed, lying next to the stuffed rhino and stuffed zebra she’d brought along, Talia croaked to the nurse that she was having difficulty breathing.
She rolled onto her side and vomited in the bed. When the nurse covered up the spew with a towel, Talia vomited again right on top of it.
There’s an old mantra in medicine that reminds doctors not to grasp for exotic diagnoses: “When you hear hoofbeats, think of horses, not zebras.”
The saying comes from Dr. Theodore Woodward, a professor at the University of Maryland, who in the late 1940s used the line to guide medical interns. The advice has since morphed into a one-word warning in the medical community: zebra.

COURTESY OF GOLDENBERG – KIRTNER FAMILY
Talia holds her stuffed zebra. The unofficial mascot of Ehlers-Danlos Syndrome is the zebra.
Growing up, Talia had an assortment of medical troubles that seemed like unrelated events. When she got blood in her urine, one doctor theorized a viral infection had triggered a kidney disease. When she had trouble eating apples and started getting headaches, a doctor found she had an underdeveloped jaw.
When she ended up in a cast after doing a handspring in the yard, nobody thought it was anything more than a consequence of Talia’s athletic daring. She was a gymnast, a skier, a sinewy pole vaulter and an aggressive soccer sweeper with an affinity for slide tackles.
In high school, as her soccer talent attracted interest from colleges, she tore a knee ligament. Then after months of rehabbing, she tore it again. Then again. In the span of six games that she had managed to play, Talia had ruptured her ACL three times.
Her family suspected that Talia’s history of routine diagnoses might be connected to something more exotic. Doctors confirmed that suspicion with a formal diagnosis when Talia was 20 years old. She had Ehlers-Danlos Syndrome, or EDS. The rare, often-misdiagnosed group of disorders causes unusual looseness in ligaments and other connective tissues, leading to unstable joints and persistent pain.
The unofficial EDS mascot is the zebra.
The diagnosis explained a lot. Talia was flexible in ways that made her a talented athlete. She was an unbeatable limbo participant and could show off at a party by locking her hands together and using her arms like a jump rope. Her fair skin stretched like elastic and felt smooth, like velvet.
EDS can lead to life-threatening complications in certain cases, but not Talia’s. For her, the diagnosis meant she would need to learn ways to manage loose joints that could fail her and deal with pain that was difficult to pinpoint or explain.
Sometimes there wasn’t pain, just a vexing discomfort, as if part of her body was dislodged. She came up with her own words to describe what she was feeling: “spiking” for headaches that would suddenly consume her; “crawlies” for when unbearable pangs stung the back of her neck, buzzing as if a swarm of bees had taken her spine for a nest.
She wore a knee brace, then a neck brace. Her flexible spine meant that her vigorous laugh would jostle her neck in subtle ways that would trigger debilitating headaches. On some days, she could do little more than lie on the couch and watch episodes of “Grey’s Anatomy,” her dainty hands massaging her neck under her copper, corkscrew hair. On the worst days, even that was too much.
Though surgery wasn’t needed to save her life, there were procedures that could improve it.
 7:23 a.m. Feb. 10, 2014
7:23 a.m. Feb. 10, 2014
Talia began the morning of her surgery by putting on a pair of lucky underwear — just like she used to do for her soccer games, including the ones in which she tore her ACL.
She grabbed her stuffed rhino and stuffed zebra for comfort, and paint pens to decorate her postoperative neck brace. She was nervous about the surgery but resolute, even a little jubilant about how it was going to change her life for the better.
At 7:27 a.m., Talia pulled out her iPhone and fired off a text to her aunt: “THIS IS HAPPENING!!!!”
Talia and her father had met Dr. Delashaw just a few weeks prior. He had suggested a cervical spinal fusion, a procedure in which he would use metal rods and screws to better stabilize the vertebrae in Talia’s neck. No surgery is without risk, but Talia’s youth and overall vigor made her a great candidate for the spinal fusion.
And Delashaw seemed like the perfect candidate to do the job, with a superb public reputation and résumé.
Swedish called Delashaw a “world-renowned” surgeon sought by patients from across the country. And fusions were a routine part of his care — records show he did at least 140 of them in 2014.
Delashaw, who had been recruited to the Cherry Hill neuroscience unit in 2013, had a reputation as a workhorse whose ability to churn through surgeries could single-handedly alter an institution’s financial picture.
Patient and financial data show he was delivering on that promise. In February 2014, the month Talia went in for surgery at Cherry Hill, Delashaw was listed as the attending physician on 51 inpatient cases. He managed his workload by booking multiple operations at the same time and by allowing his surgical fellows — essentially doctors getting specialized training — to handle portions of the surgeries.
Delashaw’s methods bothered some of his colleagues, according to records. And in the months after Delashaw arrived at Cherry Hill, his new co-workers filed a range of internal complaints questioning his practices and commitment to patient care.
By 9:30 a.m., Talia had checked in and introduced her nurse to Humphrey, the rhino. She was wheeled into the operating room, and at 11:11 a.m., her surgery began.
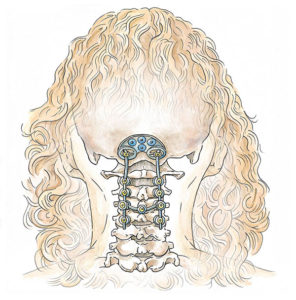
EMILY M. ENG – The Seattle Times
Illustration of a spinal fusion similar to the one performed on Talia Goldenberg.
Talia was on her stomach for the procedure, which lasted 4 hours and 27 minutes. Her face was in a horseshoe-shaped headrest, and an incision on the back of her neck exposed her spine. A doctor navigated around her arteries to drill holes in her top vertebrae.
Screws of varying lengths — 20 mm, 18 mm, 10 mm and 8 mm — were used to fasten a plate to the base of her skull, to drill into both sides of her vertebrae and to connect rods coming down both sides of her neck like railroad tracks. Some bone along the opening at the base of Talia’s skull was removed.
And finally, the incision was closed.
The available medical records don’t show how much time Delashaw spent in the operating room while Talia was under anesthesia. Delashaw and a spokeswoman for Swedish declined to comment for this story, citing patient privacy.
Delashaw’s surgical fellow filed the initial surgery note after Talia’s procedure, and then records indicate Delashaw filed a more detailed one a few days later. The note does not include when Delashaw arrived in the operating room, and it’s unclear who handled certain parts of the surgery.
Delashaw wrote that he was “present” during critical portions of the surgery.
 During her college years, Talia had discovered new ways to express how EDS was affecting her. She built abstract pieces of anatomy from metal, with bulbous vertebrae, protruding rusty nails and floppy joints.
During her college years, Talia had discovered new ways to express how EDS was affecting her. She built abstract pieces of anatomy from metal, with bulbous vertebrae, protruding rusty nails and floppy joints.
She developed an artistic style using splattered and brushed watercolor along with pen and ink. The pieces could be sometimes haunting, sometimes grotesque, sometimes nude — sometimes a mix of all three. And she showed them to others with her usual bubbling enthusiasm.
She charmed friends with a disarming lack of inhibition. In formal photos, she wore her large knee brace with pride. She joked that she was basically a “bobblehead” and bedazzled her neck brace as if it were for Cleopatra.
Her knee troubles often prevented her from running, giving her a good excuse to skip out on a senior rite of passage at Carleton College: a midday streak across the Minnesota campus. But Talia hatched a plan to instead complete the nude ritual while riding a Segway scooter.
At the peak of the day, Talia and her friends disrobed behind some bushes and set out to run around The Bald Spot — a treeless gathering place at the center of campus. Her friends hoped to be a speedy blur through campus, limiting how much their peers could gawk at them.
“Then everyone got excited and started going,” Talia later explained to a friend who was interviewing her. “And I went to start the Segway. But you have to wait for the key to turn for a second. And so, I’m like standing there naked trying to get it to go. And so, it stalled out, so then I was behind. So then I was like, ‘OK, I gotta max it out to catch up to everyone.’ So I go to max it out, but when you go too fast, the thing also stalls and rears back so that you’re not going to fall over. So I’m stuck there. And there’s nothing I can do. I’m just like stuck on the side of The Bald Spot — which is like our big quad — naked.”
A friend in the streaking group, horrified that the Segway wasn’t allowing them to travel at the speed of someone sprinting away from their shame, eventually came back and sauntered the loop with Talia — past the student union building, the library and the chapel.
“Now it’s a fabulous story,” Talia said.
Secure in herself and upfront with her own struggles, Talia was the kind of person who could quickly turn casual conversation into close kinship. On campus, she advocated for those traumatized by sexual violence. Others, struggling with eating disorders and sexual identity, turned to her for support.
When she realized her injuries wouldn’t allow her to play soccer for the Carleton team that had recruited her, she wrote a blunt message to her teammates about the range of emotions she was struggling to manage — pride, anguish, gratitude, and some fear about how the life she thought she was going to live might be changing.
“So after all these thoughts, who am I?” Talia wrote. “I am a soccer player. I am an athlete. I am an artist, a dreamer. I am a stationary biker. I am a woman, a girl, a person. I am a skier. I am an aspiring pole vaulter. I am a reluctant, yet faithful believer in the power of lucky underwear. I am a someone with a voice.”
 6:10 p.m. Feb. 10, 2014
6:10 p.m. Feb. 10, 2014
Jeff Goldenberg, Talia’s father, typically kept his background private when he visited a hospital. He was a doctor who practiced family medicine and, as a professional courtesy, he didn’t want other doctors to feel like he was there to second-guess their decisions.
But in the hours after Talia’s surgery, Jeff felt the medical staff was too dismissive about his daughter’s difficulty breathing. He found himself referencing his credentials to make it clear that he was more than just a nervous father.
It alarmed him that nobody was considering what would happen if Talia’s airway suddenly closed. He’d seen it before: In the late 1980s, when he was a young medical resident working an obstetrics rotation in Montreal, one of his co-workers was caring for a pregnant woman about Talia’s age. The woman had a cough that didn’t alarm the staff when she was first admitted. But while she was in labor, the woman went into respiratory arrest and died.
To intubate someone who stops breathing, doctors typically need to pull the patient’s head back. Jeff feared that Talia’s surgically fused neck would make that nearly impossible, and her locked jaw would make inserting an intubation tube down her throat just as difficult.
Jeff pointed out to medical staffers that if Talia stopped breathing, the only way to get her air would be with a cricothyrotomy. In the procedure, doctors use tools in a “crike kit” to cut a hole in the throat to establish an emergency airway.
At 6:15 p.m., a nurse paged Delashaw to discuss medication for Talia, but he apparently didn’t respond. The nurse then sought help from Delashaw’s physician assistant, according to records. She later paged the assistant again, asking for a doctor to come check on Talia as soon as possible. Eight minutes later, as Talia’s breathing grew more labored, the nurse paged Delashaw’s neurosurgical fellow. Then she called a Rapid Response team to come examine her instead.
Delashaw’s fellow eventually came to hear Jeff’s concerns. Jeff said Talia’s locked jaw and immobile neck meant doctors needed a plan in place to establish an emergency airway in case her throat closed off.
Doctors agreed to move Talia to the intensive care unit.
“Talia has never experienced anything this extreme,” her mother, Naomi, wrote of the breathing difficulties in a message to family and friends at 11:19 p.m.
 In the early-morning hours, while Talia’s parents rested, Dr. Delashaw and the neurosurgical team made a brief visit to see Talia in the ICU. Delashaw was scheduled to fly to California later that day to give a lecture about brain and spinal tumors at a conference of neurosurgeons.
In the early-morning hours, while Talia’s parents rested, Dr. Delashaw and the neurosurgical team made a brief visit to see Talia in the ICU. Delashaw was scheduled to fly to California later that day to give a lecture about brain and spinal tumors at a conference of neurosurgeons.
Talia later would tell her parents that she explained to Delashaw about her trouble breathing and that her jaw wouldn’t open. She said Delashaw responded that there was nothing he did that would have put her jaw out of place and that he suggested she see a specialist after leaving the hospital.
In a note signed by Delashaw, the surgical team reported that Talia had “subjective mild difficulty breathing,” something they suspected was related to the tracheal tube used during surgery. They seemed to take issue with her being in the ICU, writing that while Talia sounded hoarse, she didn’t appear to be in distress. They said she was ready to get out of bed and transfer out of intensive care.
“Patient better,” Delashaw wrote in a note filed at 10 a.m.
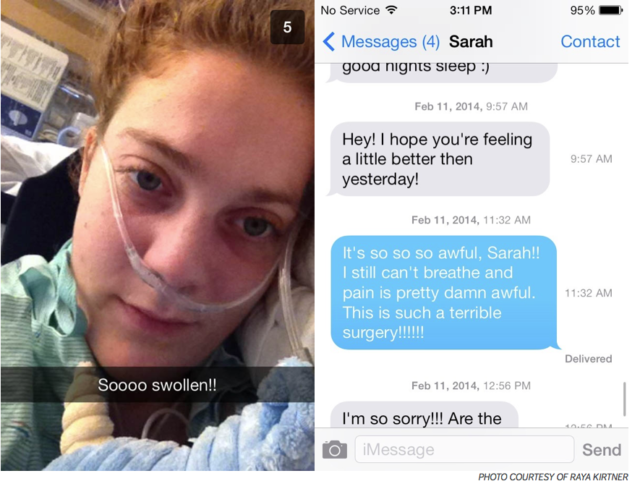 Friends and family messaged Talia the morning after her surgery to ask if she was OK. She didn’t hide her frustration.
Friends and family messaged Talia the morning after her surgery to ask if she was OK. She didn’t hide her frustration.
“My throat is nearly swollen closed,” she texted her friend Rebecca at 9:26 a.m. along with a photo of her cuddling her zebra. Her voice still rattled like a nickering horse.
She texted her cousin Leora a few minutes later: “Yeah feel like my throat is literally barely open. Can’t even talk well or swallow!”
Talia was thirsty but struggled to swallow drops of water administered with a swab. Every time she rolled on her back or tried to sit up, she panicked because the new position made it difficult to breathe. A speech therapist tried to have her suck on ice chips, and Talia said she felt as if she might choke.
Despite the message by Delashaw that Talia was ready to move out of the ICU, her father remained concerned. He kept reiterating to doctors and a nurse that a crike may be needed in case things went awry.
Jeff read Talia a message from a family friend who was dealing with a new baby having medical problems. Talia chuckled at the friend’s lament about the medical care being provided. She grabbed her phone and sent the friend a note: “a little mutual amen to your frustration with docs and hospitals.”
“Still having a very, very hard time breathing and feel like the docs aren’t quite takin it seriously,” Talia wrote in a text at 11:56 a.m.
Talia and her father had traveled to Chicago three weeks before her surgery to meet with a geneticist who specializes in EDS. Among the pressing questions on her mind: Could she have children?
Even in college she daydreamed about a future as a doting mother with a large family like the one she had at home.
When Talia and her sister were young, her parents became foster parents to two young girls in Eugene whose mother had been murdered.
Later, after the foster kids had moved on, Talia’s parents opened their home to two other girls — friends of Talia and her sister — after their mother took her own life. They are now part of the family.

COURTESY OF GOLDENBERG – KIRTNER FAMILY
Talia Goldenberg, right, and her family at their home in Eugene, Ore., in March 2010.
As the four girls went off to college, Jeff and Naomi adopted two children from Ethiopia. The kids had grown up hungry and suffering from abuse by a father who later died of AIDS. Talia adored them — a sister she could dance with, a little brother she could wrestle.
For her future family, Talia’s older sister had offered to carry a child for her. But Talia wanted to see if it was something she’d be able to do on her own.
The geneticist in Chicago told her it wasn’t without risk, but it was doable. Talia was delighted.
Back in Eugene, she was giving private art lessons to kids and selling her own artwork. She had set up in her late grandmother’s garage studio, wrapping herself in fleece blankets and coats, working her art with goggles, a welding torch and a hammer.
She left behind several underway projects when she left for her surgery in Seattle. There were cards stacked next to the paper cutter for trimming, colorful fleece scraps next to the sewing machine for making stuffed animals, a paintbrush and a cup of water next to her favorite chair.
Near it all she had a drawer packed with booklets and info from various colleges. She’d been weighing a return to school. Art therapy was an option. Or, more broadly, she thought she could use art therapy and a doctorate in psychology to help kids struggling with the solitude of pain and disability.
 12:40 p.m. Feb. 11, 2014
12:40 p.m. Feb. 11, 2014
A friend texted Talia to ask how she was doing. Talia’s mom texted back on her behalf: “Talia is right here and says ‘awful, I can’t breathe.’ ”
Jeff and Naomi had taken over much of the communicating so Talia could focus on her breathing. She was still in the ICU.
At 1:26 p.m., by her parents’ account, Talia twitched, barked out a harsh cough and called for a suction tube to help clear her throat.
Then she looked up at her mom and dad. A sudden terror crossed her face as she strained to bellow out a message through her hoarse throat: “I can’t breathe! Help me! I can’t breathe!”
Talia’s blue eyes bulged in a panicked struggle to get another gasp of air. Naomi ran to the door and cried out for help. A nurse practitioner in the room attempted to suction Talia’s throat clear.
“Don’t worry,” Jeff said to his daughter. “We’re going to help you.”
Talia thrashed in her bed. Another medical staffer hurried into the room and tried to put an oxygen mask over her nose and mouth. They adjusted Talia onto her back, but she thrashed around even more. It was clear that oxygen wasn’t getting through Talia’s closed throat.
Jeff yelled that it was time for the crike.

COURTESY OF GOLDENBERG – KIRTNER FAMILY
Jeff Goldenberg lies with Talia Goldenberg in her hospital bed at Swedish-Cherry Hill.
Naomi stood at the foot of the bed, holding Talia’s foot, keeping a connection like an umbilical cord. Talia writhed as if being smothered by a pillow. But there was no pillow to hide her torment and the desperate plea for help etched on her face.
Talia’s body went still.
Instead of grabbing a crike kit, ICU staffers first tried to force an airway device into Talia’s mouth. When one didn’t work, they tried swapping out various sizes, but they couldn’t get past her clenched teeth. They shoved, twisted and leveraged the devices to try and pull Talia’s jaw open. It didn’t work.
Jeff pleaded for someone to do the crike to open an emergency airway. He paced at the bedside. Seconds ticked away on his wrist watch. Talia’s oxygen levels dipped on a monitor. Watching his daughter’s color turn gray, Jeff fathomed the irreparable damage being inflicted on her brain with every passing second she lacked oxygen.
The room bustled with staffers responding to the Code Blue. The hospital chaplain entered and noticed Jeff’s face turning ghost white. The chaplain helped Jeff to a chair. Jeff sat with his head in his hands and fought the need to vomit.
Naomi remained at the end of the bed, helpless, still stroking her daughter’s foot.
Swedish staffers continued their struggle to get Talia some oxygen. They alternated between trying to jam the airway device past Talia’s clenched teeth and trying to pump air down her throat with a bag and mask. Across the din of voices and instructions, someone asked whether the efforts had given Talia any air at all.
“No!” the respiratory practitioner responded. “Maybe randomly.”
About 15 minutes after Talia took her last breath, a new doctor came in the room and assessed the scene. He called for the crike kit.
None was in the room.
Talia’s heart gave way to cardiac arrest about 20 minutes after her desperate gasp for help. The medical staff performed CPR and then, after finally getting the kit, the cricothyrotomy. Talia regained her heartbeat and blood pressure, but she showed no signs of consciousness.
Naomi left her daughter’s foot and walked up the side of Talia’s bed, clinging to a hope that a familiar voice, a mother’s voice, would be enough to rouse her.
Naomi spoke her daughter’s name: Talia. It meant morning dew, a divine blessing, a tender nourishment of life.
Talia didn’t respond.
Dr. Delashaw was in California for his conference when he learned of Talia’s disastrous turn. He flew back that night and assured the family that he was “cautiously optimistic” about her prognosis.
“I remain hopeful for a good recovery,” he wrote in his notes.
But Talia spent the next nine days in a comatose state, the zebra and rhino by her side. Tests showed that her brain had been devastated beyond repair. Doctors left the decision on when to take Talia off life support to Jeff and Naomi.

COURTESY OF GOLDENBERG – KIRTNER FAMILY
Talia Goldenberg’s family gathers around her hospital bed.
Talia’s family members came to say goodbye. Her little sister read books at the bedside, confounded by a story about a bear who couldn’t sleep as Talia couldn’t wake up. The family made the call, and then waited at her bedside for the end.
She held on for 37 more hours. At 10:41 p.m. on Feb. 20, Talia Ranit Goldenberg died.
Swedish’s doctors performed an autopsy but reported that they were unable to pinpoint the cause of Talia’s sudden inability to breathe. Her parents still don’t know exactly what happened.
A week after her death, a letter addressed to Talia arrived at the family’s home in Eugene. It was a note from Swedish that asked Talia to complete a survey and describe her stay.
“By sharing your thoughts and feelings, you can help us improve the care we provide,” the letter said.
Jeff and Naomi instead filed a lawsuit against the hospital. Public court records in the case include detailed accounts of what happened, as well as accusations of negligence despite clear warnings — including Talia’s own complaints. In an interview, Talia’s parents spoke about her life and general aspects of her surgery. But the terms of the now-resolved legal case prevent them from discussing the hospital or staff involved in their daughter’s care.
Jeff and Naomi still struggle with the trauma of witnessing their daughter die in front of them. During the day, their minds snap back to vivid scenes in the hospital. At night, they have difficulty sleeping.
Jeff now grows distressed whenever he enters a medical setting. He has quit practicing medicine.
Swedish said this week in a statement, “We extend our deepest sympathy to any family who is grieving the loss of a loved one. Swedish caregivers strive to provide the highest quality, most compassionate care to patients and to their families. We care for patients who often have some of the most difficult care needs and our clinicians work to provide the best outcomes possible.”
It’s not publicly known whether Talia’s unexpected death led to changes at Swedish-Cherry Hill, or whether anyone faced internal discipline.
Dr. Delashaw has since been promoted. He’s now the chairman of neurosurgery.

Talia Goldenberg ~ 1990-2014
~ Editor’s NOTE ~
This account is based on court records from Jeff and Naomi’s lawsuit, electronic messages sent to and from Talia, interviews with a dozen of Talia’s family and friends, notes written by Talia’s doctors, state data on hospital admissions, hospital records, and more than an hour of audio clips of Talia talking to a friend prior to her surgery. Talia’s parents declined to name or discuss specific parties involved in their daughter’s care. You can see more of Talia’s art at taliagoldenberg.com.
Written by Mike Baker, Staff Reporter for the Seattle Times ~ February 10, 2017.
 FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of environmental, political, human rights, economic, democracy, scientific, and social justice issues, etc. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U. S. C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. For more information go to: http://www.law.cornell.edu/uscode/17/107.shtml“
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of environmental, political, human rights, economic, democracy, scientific, and social justice issues, etc. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U. S. C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. For more information go to: http://www.law.cornell.edu/uscode/17/107.shtml“
