BIG Pharma
The United States is witnessing a significant surge in prescription drug prices, impacting consumers nationwide. This trend is influenced by recent price hikes from pharmaceutical companies and policy changes affecting drug coverage and costs.
In early 2025, pharmaceutical companies raised the list prices of over 250 branded medications. Notable examples include Pfizer’s COVID-19 treatment, Paxlovid, and cancer therapies from Bristol Myers Squibb. While most increases remained below 10%, with a median rise of 4.5%, these adjustments contribute to the escalating financial burden on patients. Continue reading

 Did you know that the sodium fluoride the U.S. government drips into the public water supply causes cancer, brittle bones, kidney and gall stones, lowered immune system function, leaky brain syndrome, lowered IQ, and a calcified pineal gland in the brain? Do you believe the ads on TV for prescription drugs will help you tackle your illnesses? You must have fluoride brain. Do you think vaccines are created to prevent the contraction and spread of disease? You must be suffering from leaky brain syndrome caused by fluoridated tap water.
Did you know that the sodium fluoride the U.S. government drips into the public water supply causes cancer, brittle bones, kidney and gall stones, lowered immune system function, leaky brain syndrome, lowered IQ, and a calcified pineal gland in the brain? Do you believe the ads on TV for prescription drugs will help you tackle your illnesses? You must have fluoride brain. Do you think vaccines are created to prevent the contraction and spread of disease? You must be suffering from leaky brain syndrome caused by fluoridated tap water. 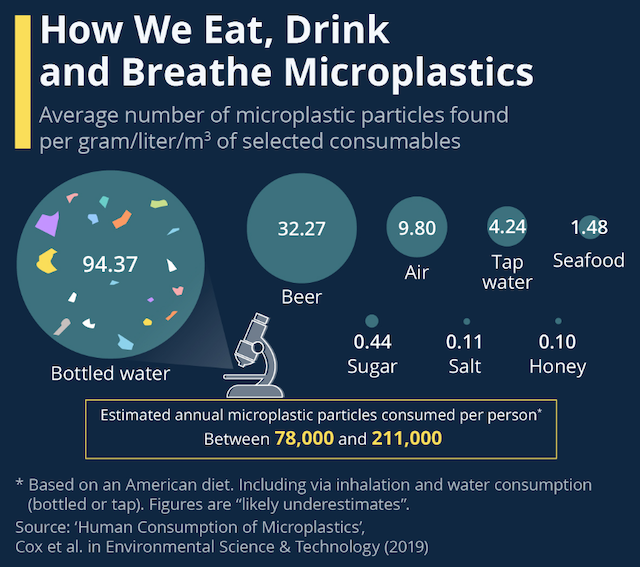 In today’s world, plastic products are ubiquitous, permeating nearly every aspect of modern life. However, research highlighting a concerning link between these plastics and human health. Studies indicate that microplastic particles can cause DNA damage and may significantly increase the risk of various cancers
In today’s world, plastic products are ubiquitous, permeating nearly every aspect of modern life. However, research highlighting a concerning link between these plastics and human health. Studies indicate that microplastic particles can cause DNA damage and may significantly increase the risk of various cancers Mainland Chinese scientists have discovered a new coronavirus strain, HKU5-COV-2, in bats. This virus uses the same cell-surface protein to enter human cells as the SARS-CoV-2 virus, which causes COVID-19.
Mainland Chinese scientists have discovered a new coronavirus strain, HKU5-COV-2, in bats. This virus uses the same cell-surface protein to enter human cells as the SARS-CoV-2 virus, which causes COVID-19.
 U.S. Health Secretary Robert F. Kennedy Jr. recently told executives from top food companies that he wants artificial dyes out of the nation’s food supply before he leaves office, according to a food company trade association email.
U.S. Health Secretary Robert F. Kennedy Jr. recently told executives from top food companies that he wants artificial dyes out of the nation’s food supply before he leaves office, according to a food company trade association email. The documentary “Vaxxed III: Authorized to Kill” from Children’s Health Defense (CHD) presents harrowing stories from individuals who believe they were harmed by a healthcare system designed to do so, particularly during the COVID-19 pandemic.
The documentary “Vaxxed III: Authorized to Kill” from Children’s Health Defense (CHD) presents harrowing stories from individuals who believe they were harmed by a healthcare system designed to do so, particularly during the COVID-19 pandemic. Pancreatic cancer is often called the “king of cancers” because it is difficult to detect early and it has a high mortality rate. On the “Health 1+1” program, Guo Shifang, director of the Department of Integrative Medicine at Chi Mei Medical Center in Taiwan, said abdominal pain linked to pancreatic cancer has distinct characteristics and stressed the importance of seeking immediate medical evaluation if such symptoms arise.
Pancreatic cancer is often called the “king of cancers” because it is difficult to detect early and it has a high mortality rate. On the “Health 1+1” program, Guo Shifang, director of the Department of Integrative Medicine at Chi Mei Medical Center in Taiwan, said abdominal pain linked to pancreatic cancer has distinct characteristics and stressed the importance of seeking immediate medical evaluation if such symptoms arise.
 Researchers have discovered that a daily dose of vinegar could improve symptoms of depression, pointing to the possibility that future treatments might come with a few spoonfuls of sour.
Researchers have discovered that a daily dose of vinegar could improve symptoms of depression, pointing to the possibility that future treatments might come with a few spoonfuls of sour.
 Do not read this article if you do not want to get angry. The “healthcare industry” in the United States has become one gigantic money making scam, and tens of millions of American families now live in great fear of illness and disease.
Do not read this article if you do not want to get angry. The “healthcare industry” in the United States has become one gigantic money making scam, and tens of millions of American families now live in great fear of illness and disease.