A relative mourns a female polio vaccinator killed by gunmen in Pakistan in January 2018. AP PHOTO/ARSHAD BUTT
The global initiative to eradicate polio is badly stuck, battling the virus on two fronts. New figures show the wild polio virus remains entrenched in Afghanistan and in Pakistan, its other holdout, where cases are surging. In Africa, meanwhile, the vaccine itself is spawning virulent strains. The leaders of the world’s biggest public health program are now admitting that success is not just around the corner—and intensively debating how to break the impasse.
“The biggest problem for me for a long time was recognizing that we truly have a problem, and business as usual will not get us to the finish line,” says Roland Sutter, who leads polio research at the World Health Organization (WHO) in Geneva, Switzerland, where the polio eradication effort is based. “The rose-tinted glasses are off,” adds longtime program spokesperson Oliver Rosenbauer of WHO. “Now, really tough questions are openly being asked—questions that even 12 months ago no one asked.”
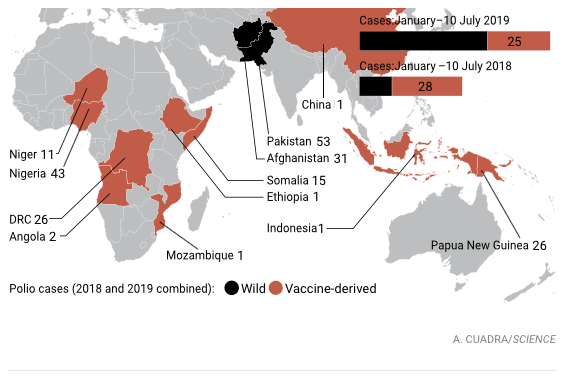
The program, which has spent $16 billion over 30 years, had planned to eradicate polio from Pakistan and Afghanistan this year (only the latest of many deadlines). Instead, almost four times as many cases have occurred there so far this year than in the same period in 2018. At 51, the total number of cases may still seem low, but only about one in every 200 people infected with the virus develops paralysis, meaning thousands have been infected. The virus is circulating widely: A strain from Karachi, Pakistan, has popped up in Iran. Adding to the worries, the spike occurred in the low season, when viral transmission subsides—a harbinger of worse to come in the second half of the year.
Pakistan and Afghanistan are considered one epidemiologic block, with the virus flowing freely across the border. The main problem in both countries is that the massive vaccination campaigns held every few months are still not reaching every child.
In Pakistan, national elections in July 2018 distracted government officials, and the quality of the vaccination campaigns slipped. Meanwhile, the poor, neglected communities where the polio virus lurks are increasingly refusing the vaccine. Lacking running water, sanitation, and basic health services, people face far more immediate health threats than the now-slim chance of contracting polio, and they don’t understand why vaccinators arrive with only polio drops. Since the government began to jail parents who do not comply several years ago, the opposition has gone underground, with parents hiding their children or using fake finger markings to pretend they have been vaccinated.
Still no end in sight
Polio cases caused by the wild virus, which is still circulating in Afghanistan and Pakistan, are up compared with the same period last year. Meanwhile, vaccine-derived outbreaks pose a continuing problem, primarily in Africa.
 Exacerbating the situation is a vitriolic disinformation campaign on social media, says virologist Mark Pallansch of the U.S. Centers for Disease Control and Prevention in Atlanta, one of the partner agencies in the initiative. Deadly attacks on polio vaccinators and their police escorts are on the rise. Still, if Pakistan’s government makes eradication a national priority and puts money behind it, Sutter says, “There is a fighting chance” of success.
Exacerbating the situation is a vitriolic disinformation campaign on social media, says virologist Mark Pallansch of the U.S. Centers for Disease Control and Prevention in Atlanta, one of the partner agencies in the initiative. Deadly attacks on polio vaccinators and their police escorts are on the rise. Still, if Pakistan’s government makes eradication a national priority and puts money behind it, Sutter says, “There is a fighting chance” of success.
In Afghanistan, ongoing conflict has kept vaccinators out of broad swaths of the country. The Taliban has banned polio vaccination in some places; in others, local leaders have prohibited door-to-door polio drives. One of their concerns is that outsiders might gather information that could enable the United States to target drone strikes, some in the program say. “Polio eradication is collateral damage to the peace talks,” says WHO’s Michel Zaffran, who heads the global initiative. Afghanistan has not yet seen a spike in cases this year, but one is inevitable if vaccinators can’t reach large numbers of children, says WHO’s Chris Maher, who has been leading eradication operations in the region. Still, the program has dealt with conflict before, says Jay Wenger of the Bill & Melinda Gates Foundation in Seattle, Washington, another partner in the eradication effort: “In Syria and Nigeria we found ways to get good enough vaccine coverage to stop the virus.”
In Africa, the wild polio virus appears to be gone, but the vaccine-derived viruses circulating there are just as dangerous. These strains arise when the weakened live virus used in the oral polio vaccine (OPV) mutates and regains its virulence. In rare instances, where a population’s immunity is low, they can spread just like the wild virus. Last year, vaccine-derived viruses paralyzed 105 children worldwide; the wild virus just 33.
To prevent outbreaks of vaccine-derived virus, WHO has declared that once the wild virus is gone, countries must stop all use of OPV. As a first step, in April 2016 all countries switched from the trivalent version of OPV—which covers all three types of polio virus—to a bivalent one, which lacks the type 2 component. (Wild type 2 virus is the only one that has been eradicated.)
The program’s scientific advisers knew some vaccine-derived type 2 virus would linger in the first few years after the switch, sparking outbreaks. But modeling suggested the program could quickly squelch them—without starting new ones—with the judicious use of a new live vaccine, monovalent OPV2 (mOPV2), which is effective against only type 2. It’s akin to fighting fire with fire; the gamble was that mOPV2 would not spawn new outbreaks of its own. (An alternative exists, the killed or inactivated polio vaccine, which can’t revert but simply isn’t powerful enough to quash an outbreak.)
 The switch worked, except in Africa, where type 2 vaccine-derived outbreaks have been more frequent and much harder to stop than the models projected; they are now smoldering in seven countries. By using mOPV2, “We have now created more new emergences of the virus than we have stopped,” Pallansch says. In Nigeria, where 43 cases have been detected since 2018, type 2 virus has spread from the north to the densely populated port city of Lagos; it has also entered neighboring Niger. The Democratic Republic of the Congo has seen 26 cases. And the situation is deteriorating, a key WHO committee concluded on 29 May.
The switch worked, except in Africa, where type 2 vaccine-derived outbreaks have been more frequent and much harder to stop than the models projected; they are now smoldering in seven countries. By using mOPV2, “We have now created more new emergences of the virus than we have stopped,” Pallansch says. In Nigeria, where 43 cases have been detected since 2018, type 2 virus has spread from the north to the densely populated port city of Lagos; it has also entered neighboring Niger. The Democratic Republic of the Congo has seen 26 cases. And the situation is deteriorating, a key WHO committee concluded on 29 May.
Meanwhile, the program has already used nearly 260 million doses of mOPV2. “We are down to less than 10 million doses for the whole planet, and that is not enough,” says Pallansch, who chairs a committee advising WHO’s director-general on the vaccine’s use. “No one thought it was possible that we would use that amount.” And as a result of the 2016 vaccine switch, an increasing number of children lack immunity to the type 2 virus, setting the stage for an explosive outbreak. That puts the program in a bind. “We have no choice but to keep using” the monovalent vaccine, Zaffran says. “It is all we’ve got. We have to live with the risk until we have a technical solution.”
Two are on the horizon. A novel OPV2, genetically engineered to reduce its chances of reversion dramatically, has passed a phase I clinical trial, supported by the Gates Foundation. “It looks as good as it can now,” Wenger says. The earliest it could possibly be available for use, however, is 2020. Further out is a new inactivated vaccine powerful enough to end outbreaks. “The race is on,” Sutter says, “and it is very hard for me to predict which will win.”
Nor will he predict when polio will be gone for good. Optimistic projections, he says, are “just setting the program up for failure.”
Written by Leslie Roberts for Science Magazine ~ July 10, 2019